Once biopsy and other investigations are concluded; Doctors categorize prostate cancer stages from 1 (mild) to Stage 4 prostate cancer (severe). It’s significant to learn the stage (location) and grade (aggressiveness) of the tumor

Thought it appears accommodating, there are threats:
I. It could scare the patient into taking much more aggressive action for treatment than is not necessary.
II. Alternatively it could make the doctor push you in a more proactive and aggressive "preventative" action by performing a radical prostectomy, the removal of your prostate gland.
III. Most prostate cancers are best left alone than to be treated with modern methods of surgery, radiation or hormone or drug chemo methods.

Why?
Because most cases of prostate cancer stages are usually the milder versions well contained in the prostate gland and are very slow growing. Most men will die of something else than their prostate cancer. So often the recommendation is "watchful waiting". But if you are younger, then you or your doctor may be tempted to try more aggressive approaches no matter what stages of prostate cancer you are experiencing. But please learn more about your prostate gland functions before you do that because you will then have a life of possible serious side effects: incontinence (common), erectile difficulties (also common) and perhaps a painful rectum. The prostate is too significant organ to dismiss it so readily.
Making an educated treatment decision begins with the stage, or progression, of the disease. When you are diagnosed with prostate cancer; ask of the stage of the cancer from the doctor and know the treatment options available before taking the decision. Knowing your stage you can then take the decision
Medical treatment options include:
i. Radical prostatectomy (prostate removal)
ii. External beam radiation
iii. (implanting radiation seeds)
iv. Brachytherapy plus external beam radiation combined
v. Cryosurgery (surgery to freeze cancerous tissues)
vi. Hormone treatment
Staging?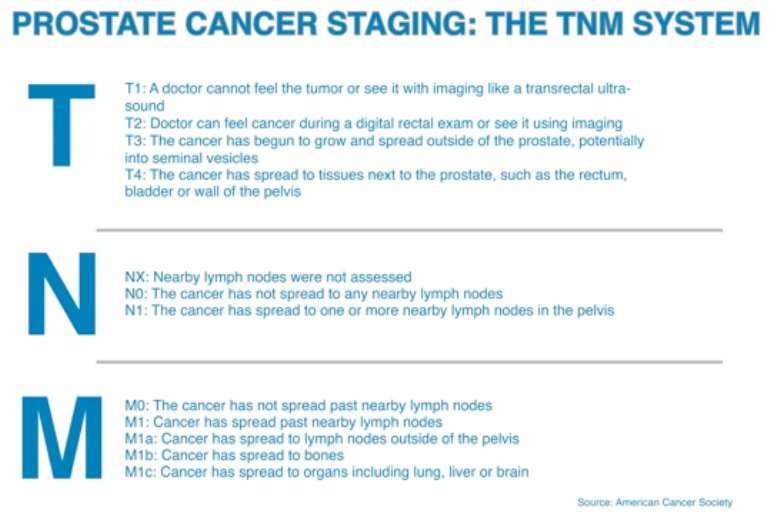
Staging is the process used to find out if the cancer has spread within the prostate or to other parts of the body, using biopsy and imaging.
Classifications
Stage I prostate cancer
In stage I, the cancer is confined to the prostate. Stage I can’t be detected during a digital rectal exam (DRE). It is usually expected to be slow growing.
Stage II prostate cancer
With stage II, cancer can be detected during a DRE. It’s still confined to the prostate, but the cells may be more abnormal and may grow faster.
Stage III prostate cancer
With stage III prostate cancer, the cancer is in tissues near the prostate. It also may have reached the seminal vesicles.
Stage IV prostate cancer
Stage IV prostate cancer means that cancer has invaded other parts of the body, such as the rectum, nearby lymph nodes or bone. Stage 4 prostate cancers are classified as the stage where the cancer has progressed and spread to other tissues outside the prostate, leading to metastatic cancer. It can take many years for the cancer to reach this stage and early signs of prostate cancer would have been visible long beforehand, signaling a change in lifestyle and a healthier diet was in order. However, if you believe you may have stage 4/metastatic cancer it is important to know what options are available and what to do.

Symptoms of Stage 4 Prostate Cancer
If the prostate cancer has spread, become more severe and moved to a stage 4 then you might also experience the following symptoms:
Bone pain, especially around the hips, thighs and lower back
Swelling of the feet and legs
Weight loss
Fatigue
Significance of staging and grading for treatment
These two numbers are the most important for determining your future course of treatment. Some treatments are only effective for Stages I and II, where the cancer is still confined to the prostate. Some other treatments only become necessary at Stages III and IV, where the cancer has spread outside the prostate.
Grading is especially useful in early-stage disease. If the tumor shows signs of being aggressive, it may make sense to go forward with treatment. If the tumor does not seem aggressive, it may make sense to go forward with active surveillance and avoid side effects.
In any case, the stage and grade should be a vital component of any discussion with your doctor.

Detail on staging
The standardized Tumor, Node, and Metastasis (TNM) system is used to stage prostate cancer. The T category is based on the extent of the tumor itself. The N category is based on whether the cancer has spread to nearby lymph nodes. The M category is based on whether the cancer has spread beyond nearby lymph nodes.
T (Tumor) Categories:
T1: the tumor cannot be felt with a DRE or seen with imaging
T1a: the tumor is found accidentally during a surgery for benign prostatic hyperplasia or another prostate condition. The tumor takes up less than 5% of the removed tissue
T1b: the tumor is found accidentally during a surgery, and the tumor takes up more than 5% of the removed tissue

T1c: the tumor is diagnosed with a needle biopsy, usually because of an elevated PSA
T2: the tumor is confined to the prostate and can be either felt with a DRE or seen with imaging
T2a: the tumor is confined to half of one lobe of the prostate
T2b: the tumor is present to more than half of one lobe, but is not in both lobes
T2c: the tumor is present in both lobes of the prostate
T3: the tumor has grown outside of the prostate and may be present in the seminal vesicles
T3a: the tumor is outside of the prostate, but is not in the seminal vesicles
T3b: the cancer is outside of the prostate and has spread to the seminal vesicles
T4: the tumor has grown into tissues beyond the seminal vesicles
N (Node) Categories:
NX: nearby lymph nodes were not checked for cancer
N0: the tumor is not present in nearby lymph nodes
N1: the tumor has spread to one or more nearby lymph nodes
M (Metastasis) Categories:
M0: the cancer is not present in other parts of the body beyond the nearby lymph nodes
M1: the cancer is present in the body beyond the nearby lymph nodes
M1a: the cancer has spread to distant lymph nodes
M1b: the cancer has spread to the bones
M1c: the cancer has spread to other organs
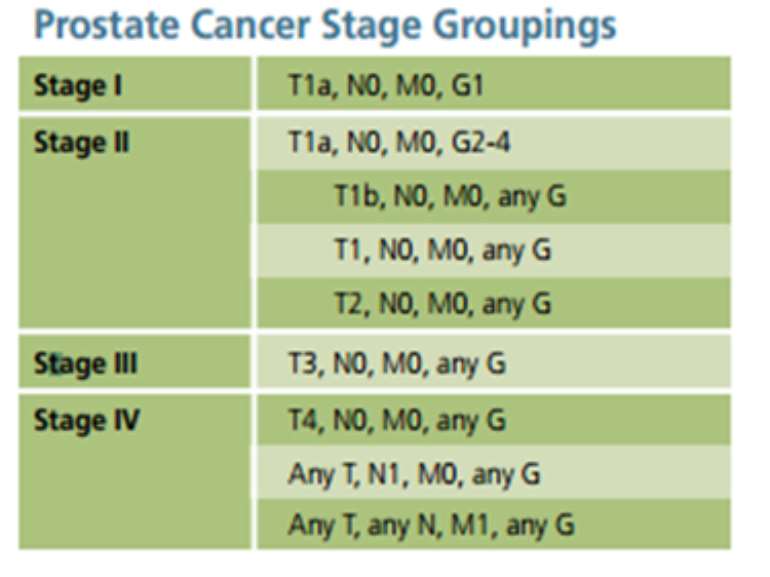
Each of the stages is based on some combination of these categories.
Stage 1:
The tumor cannot be felt with a DRE or seen with imaging (T1), and the PSA is less than 10 ng/mL, with a Gleason score of 6 or lower; OR
The tumor can be felt with a DRE or seen with imaging, but is confined to half of one lobe (T2a), and the PSA is less than 10 ng/mL, with a Gleason score of 6 or lower; OR
The tumor is either in T1 or T2a, but the PSA and Gleason score are unknown
Stage 2A:
The tumor cannot be felt with a DRE or seen with imaging (T1), or the tumor is confined to half of one lobe (T2a), and the PSA is less than 20 ng/mL, with a Gleason score of 7; OR
The tumor is either in T1 or T2a, and the PSA is equal or more than 10 ng/mL but less than 20 ng/mL, with a Gleason of 6 or lower; OR
The tumor is present to more than half of one lobe, but is not in both lobes (T2b), and the PSA is less than 20 ng/mL, with a Gleason score of 7 or lower; OR
The tumor is present to more than half of one lobe, but is not in both lobes (T2b), and the PSA and Gleason score are unknown
Stage 2B:
The tumor is present in both lobes of the prostate (T2c), with any PSA and any Gleason score; OR
The tumor is either in T1 or T2, and the PSA is equal or less to 20 ng/mL, with any Gleason score; OR
The tumor is either in T1 or T2, with any PSA and a Gleason of 8 or higher
Stage 3:
The tumor has grown outside of the prostate and may be present in the seminal vesicles (T3), with any PSA and any Gleason score
Stage 4:
The tumor has grown into tissues beyond the seminal vesicles, with any PSA and any Gleason score, OR
The tumor has spread to one or more nearby lymph nodes, without metastases, with any PSA and any Gleason score; OR
The cancer is present in the body beyond the nearby lymph nodes, in tissues like the bone or distant organs, with any PSA and any Gleason score

What are the D’Amico risk categories?
The D’Amico system provides an estimate of the risk of recurrence at five years after treatment. This system is one of the most widely used for risk assessment. It combines the PSA, Gleason score, and the clinical stage to create low, intermediate, and high risk categories. The higher the risk category, the higher the chance of recurrence is five years after treatment.
The D’Amico risk categories are below. If one factor is putting you in a lower category but another is putting you in a higher category, then the higher category takes precedent.
Low Risk:
PSA is less than 10 ng/mL AND
Gleason score is equal to or less than 6 AND
Clinical stage T1-T2a
Intermediate Risk:
PSA is between 10 and 20 ng/mL OR
Gleason score is 7 OR
Clinical stage T2b
High Risk:
Gleason score is 8-10 OR
PSA is greater than 20 ng/mL OR
Clinical stage T2c-T3

Treatment Options
If you are displaying the symptoms above it is important not to panic and to carefully think about the options available to you. Discovering your prostate cancer is at Stage 4 or is metastatic cancer can be difficult to deal with but it is essential to carefully think about the next step you take.
Many men will rush to the doctor, who in turn will suggest undertaking surgery or chemotherapy or both, which brings new dangers.
Surgery itself can cause prostate cancer metastasis, which is a further spreading of the cancer outside the prostate.
Chemotherapy is capable of causing Stage 4 prostate cancer to spread even further and to aggravate the cancer. Recent studies have concluded that toxic drugs, such as the ones used in chemotherapy, suppress tumor growth on one cell population while initiating growth in another. This can leave you requiring treatment for the rest of your life and can be a painful route to take both emotionally and physically.

Recurrent prostate cancer
About 45% of prostate cancers recur. Prostate cancer treatments are designed to kill cancerous cells, but sometimes, malignant cells remain in the prostate. Recurrent prostate cancer occurs when the cancer has returned after treatment. The malignancy may recur in the prostate area or in other areas of the body.
Cancer that returns to the prostate is called a local recurrence. If the disease develops in another part of the body, it is called metastatic prostate cancer, regional recurrence or distant recurrence. Cancer cells may travel away from the original prostate tumor to other parts of the body through the blood or lymphatic system. If the cancer metastasizes or spreads outside the prostate, it most likely develops in nearby lymph nodes first and then travels to the bones. The cancer may also spread to the liver or other organs.
It is important to report any new signs or symptoms to your doctor. Symptoms of recurrent prostate cancer vary from person to person. Depending on its size and location, a prostate tumor may press on and constrict the urethra, causing a variety of urinary symptoms.

Signs and symptoms of local prostate cancer recurrence may include:
Burning or pain during urination
Difficulty urinating, or trouble starting and stopping while urinating
More frequent urges to urinate at night
Loss of bladder control
Decreased flow or velocity of urine stream
Blood in urine (hematuria)
Signs and symptoms of metastatic prostate cancer may include:
Erectile dysfunction or painful ejaculation
Swelling in the legs or pelvic area
Numbness or pain in the hips, legs or feet
Bone pain that does not go away or leads to fractures
The symptoms of prostate cancer often differ from patient to patient. The most common first sign of recurrent prostate cancer is a rise in the level of prostate specific antigen (PSA) in the blood, making regular PSA tests all the more important in measuring the progress of treatment and checking for signs of recurrence.
Measuring the prostate cancer recurrence rate is difficult because risk factors vary widely from patient to patient. Prostate cancer recurrence risk factors include PSA level, Gleason score and the cancer’s latest stage. If your prostate has been removed, it may be tested to offer details about the aggressiveness of the cancer and your risk of recurrence. Stay blessed. Enquiries call 0541234556...Do you know the PSA is also found in women? Next week all you need to know about the PSA Test.




 2024 elections: Resign if you can't be faithful to party - Sagnarigu NDC PC desc...
2024 elections: Resign if you can't be faithful to party - Sagnarigu NDC PC desc...
 Five arrested, remanded over alleged murder of two police officers at Transacco
Five arrested, remanded over alleged murder of two police officers at Transacco
 Tax exemptions better than incentives for churches – Tax Analyst tell Bawumia
Tax exemptions better than incentives for churches – Tax Analyst tell Bawumia
 Transport Minister sues Law Platform Editor for defamation
Transport Minister sues Law Platform Editor for defamation
 Voter registration: Police arrest NPP Treasurer for Mpohor for registering minor
Voter registration: Police arrest NPP Treasurer for Mpohor for registering minor
 "This nonsense must stop" — Lawrence Tetteh vows to march to Jubilee House over ...
"This nonsense must stop" — Lawrence Tetteh vows to march to Jubilee House over ...
 2024 elections: “If indeed you stand for peaceful elections the time is now for ...
2024 elections: “If indeed you stand for peaceful elections the time is now for ...
 I have the attributes to be president of this country — Bernard Monarh
I have the attributes to be president of this country — Bernard Monarh
 Cecilia Dapaah saga: ‘Turf war’ between AG, EOCO, OSP indicates they’re not ‘cor...
Cecilia Dapaah saga: ‘Turf war’ between AG, EOCO, OSP indicates they’re not ‘cor...
 Ghana will become the first African country to embrace blockchain-powered gover...
Ghana will become the first African country to embrace blockchain-powered gover...
