The prostate is a walnut-shaped gland that is part of the male reproductive system. The main function of the prostate is to make a fluid that goes into semen. Prostate fluid is essential for a man's fertility. The gland surrounds the urethra at the neck of the bladder. The bladder neck is the area where the urethra joins the bladder. The bladder and urethra are parts of the lower urinary tract. The prostate has two or more lobes, or sections, enclosed by an outer layer of tissue, and it is in front of the rectum, just below the bladder. The urethra is the tube that carries urine from the bladder to the outside of the body. In men, the urethra also carries semen out through the penis.
If you're like many adult men, you've thought about your prostate health at some point in your life. It's an important issue because 90 percent of men experience some kind of problem with their prostate by the time they are 70 years old. And one of these problems is prostatitis.
Prostatitis is a common condition that involves inflammation or an infection of the prostate gland. It's estimated that prostatitis symptoms affect 35 to 50 percent of men during their lifetime. And unlike an enlarged prostate and prostate cancer, in one article authored by Jon Rees et al 2015 and published in the BJU titled “Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline”, prostatitis affects men of all ages, especially those between the ages of 20 and 40.
The severity of symptoms vary, but most men with prostatitis suffer from painful urination; pain in the pelvic area, groin and lower back; flu-like symptoms; and issues during intercourse, such as painful ejaculation and erectile dysfunction. Thankfully, there are natural and safe ways to relieve prostatitis symptoms that will help you to feel like yourself again.
What Is Prostatitis?
The term prostatitis describes a combination of infectious diseases that involve the prostate gland. There are four categories of prostatitis:
Acute bacterial prostatitis: Acute bacterial prostatitis is estimated to comprise up to 10 percent of all prostatitis diagnoses, making it the least common form of the condition. In one article by Timothy J. Coker, And Daniel M. Dierfeldt(2016) published in the American Family Physician, postulated that, It most commonly affects men between the ages of 20 and 40 and those older than 70 years.
Chronic bacterial prostatitis: Chronic bacterial prostatitis involves recurring infections in the prostate and urinary symptoms that come and go for many months. When a bacterial infection in the prostate isn't completely eliminated, prostatitis symptoms can recur and become difficult to treat.
Chronic prostatitis/chronic pelvic pain syndrome: Chronic prostatitis is the most common and least understood form of prostatitis, making up 90 percent of cases. It is estimated to affect 10 to 15 percent of men in the United States and it can occur at any age. According to the my.clevelandclinic.org, chronic prostatitis is when there's pelvic pain and other symptoms of prostatitis, but bacteria doesn't cause it.
Asymptomatic inflammatory prostatitis: Asymptomatic inflammatory prostatitis involves inflammation of the prostate gland. The only symptom of this type of prostatitis is the presence of white blood cells in the prostate fluid; in fact, this type is usually diagnosed incidentally only after the evaluation of infertility or prostate cancer.
Signs & Symptoms
Prostatitis symptoms depend on the type and cause of the condition. Symptoms can vary from person to person.
The symptoms of acute and chronic bacterial prostatitis are similar, but the chronic form is usually not as severe. Symptoms of acute bacterial prostatitis tend to come on suddenly, while chronic bacterial prostatitis typically develops slowly and lasts for three or more months. According to the National Institute of Diabetes and Digestive and Kidney Diseases Health Information Center, The symptoms of both forms generally include:
- fever and chills (more common with acute bacterial prostatitis)
- nausea and vomiting
- frequent urination
- an urgent need to urinate
- difficulty urinating
- less powerful urine stream
- pain or burning during urination
- pain in the genital and groin area
- lower abdomen and lower back pain
- pain during ejaculation or sexual intercourse
Symptoms associated with chronic bacterial prostatitis may be persistent and mild, or they may come and go. Two potential complications of prostatitis caused by a bacterial infection are urosepsis and septicemia. Urosepsis is a severe infection of the urinary tract or the prostate that can lead to multi-organ dysfunction. Septicemia is blood poisoning by bacteria that can progress to septic shock according to Om Prakash Kalra and Alpana Raizada (2009) published in the journal Global Infectious Diseases titled “Approach to a Patient with Urosepsis”
Chronic pelvic pain involves discomfort that lasts for three months or longer. With chronic prostatitis/chronic pelvic pain, the pain may come on suddenly or develop gradually. It may also come and go for several months. Common symptoms of this type of prostatitis include:
- pain between the scrotum and anus
- pain or discomfort in the penis and scrotum
- lower back and lower abdomen pain
- pain during or after ejaculation
- pain during sexual intercourse
- pain in the urethra and/or penis during or after urination
- frequent need to urinate, up to 8–10 times a day
- urgent need to urinate and an inability to delay urination
- interrupted or weak urine stream due to prostate swelling
- impotence
Men with asymptomatic inflammatory prostatitis don't have symptoms and this type does not cause complications. It's usually detected when the patient is tested for a urinary tract infection or reproductive tract disorder.
Complications of prostatitis
The complications of prostatitis may include according to the National Institute of Diabetes and Digestive and Kidney Diseases Health Information Center:
- bacterial infection in the bloodstream
- prostatic abscess—a pus-filled cavity in the prostate
- sexual dysfunction
- inflammation of reproductive organs near the prostate
How is prostatitis diagnosed?
A health care provider diagnoses prostatitis based on
- a personal and family medical history
- a physical exam
- medical tests
A health care provider may have to rule out other conditions that cause similar signs and symptoms before diagnosing prostatitis.
Personal and Family Medical History
Taking a personal and family medical history is one of the first things a health care provider may do to help diagnose prostatitis.
Physical Exam
A physical exam may help diagnose prostatitis. During a physical exam, a health care provider usually
- examines a patient's body, which can include checking for
- discharge from the urethra
- enlarged or tender lymph nodes in the groin
- a swollen or tender scrotum
- performs a digital rectal exam
A digital rectal exam, or rectal exam, is a physical exam of the prostate. To perform the exam, the health care provider asks the man to bend over a table or lie on his side while holding his knees close to his chest. The health care provider slides a gloved, lubricated finger into the rectum and feels the part of the prostate that lies next to the rectum. The man may feel slight, brief discomfort during the rectal exam. A health care provider usually performs a rectal exam during an office visit, and the man does not need anesthesia. The exam helps the health care provider see if the prostate is enlarged or tender or has any abnormalities that require more testing.
Many health care providers perform a rectal exam as part of a routine physical exam for men age 40 or older, whether or not they have urinary problems.

Medical Tests
A health care provider may refer men to an urologist—a doctor who specializes in the urinary tract and male reproductive system. An urologist uses medical tests to help diagnose lower urinary tract problems related to prostatitis and recommend treatment. Medical tests may include
- urinalysis
- blood tests
- urodynamic tests
- cystoscopy
- transrectal ultrasound
- biopsy
- semen analysis
Urinalysis. Urinalysis involves testing a urine sample. The patient collects a urine sample in a special container in a health care provider's office or a commercial facility. A health care provider tests the sample during an office visit or sends it to a lab for analysis. For the test, a nurse or technician places a strip of chemically treated paper, called a dipstick, into the urine. Patches on the dipstick change color to indicate signs of infection in urine.
The health care provider can diagnose the bacterial forms of prostatitis by examining the urine sample with a microscope. The health care provider may also send the sample to a lab to perform a culture. In a urine culture, a lab technician places some of the urine sample in a tube or dish with a substance that encourages any bacteria present to grow; once the bacteria have multiplied, a technician can identify them.
Blood tests. Blood tests involve a health care provider drawing blood during an office visit or in a commercial facility and sending the sample to a lab for analysis. Blood tests can show signs of infection and other prostate problems, such as prostate cancer.
Urodynamic tests . Urodynamic tests include a variety of procedures that look at how well the bladder and urethra store and release urine. A health care provider performs urodynamic tests during an office visit or in an outpatient center or a hospital. Some urodynamic tests do not require anesthesia; others may require local anesthesia. Most urodynamic tests focus on the bladder's ability to hold urine and empty steadily and completely and may include the following:
- uroflowmetry, which measures how rapidly the bladder releases urine
- postvoid residual measurement, which evaluates how much urine remains in the bladder after urination
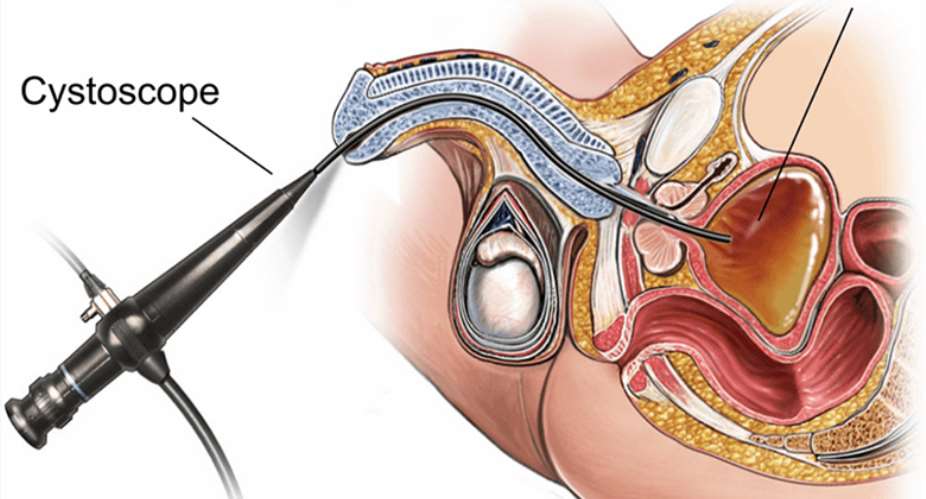
Cystoscopy . Cystoscopy is a procedure that uses a tubelike instrument, called a cystoscope, to look inside the urethra and bladder. A urologist inserts the cystoscope through the opening at the tip of the penis and into the lower urinary tract. He or she performs cystoscopy during an office visit or in an outpatient center or a hospital. He or she will give the patient local anesthesia. In some cases, the patient may require sedation and regional or general anesthesia. A urologist may use cystoscopy to look for narrowing, blockage, or stones in the urinary tract.

Transrectal ultrasound . Transrectal ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. The health care provider can move the transducer to different angles to make it possible to examine different organs. A specially trained technician performs the procedure in a health care provider's office, an outpatient center, or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images; the patient does not require anesthesia. Urologists most often use transrectal ultrasound to examine the prostate. In a transrectal ultrasound, the technician inserts a transducer slightly larger than a pen into the man's rectum next to the prostate. The ultrasound image shows the size of the prostate and any abnormalities, such as tumors. Transrectal ultrasound cannot reliably diagnose prostate cancer.

2010, when I graduated from Radford University College Medical Sonography program, my first ultrasound Machine
Biopsy. Biopsy is a procedure that involves taking a small piece of prostate tissue for examination with a microscope. An urologist performs the biopsy in an outpatient center or a hospital. He or she will give the patient light sedation and local anesthetic; however, in some cases, the patient will require general anesthesia. The urologist uses imaging techniques such as ultrasound, a computerized tomography scan, or magnetic resonance imaging to guide the biopsy needle into the prostate. A pathologist—a doctor who specializes in examining tissues to diagnose diseases—examines the prostate tissue in a lab. The test can show whether prostate cancer is present.
Semen analysis. Semen analysis is a test to measure the amount and quality of a man's semen and sperm. The man collects a semen sample in a special container at home, a health care provider's office, or a commercial facility. A health care provider analyzes the sample during an office visit or sends it to a lab for analysis. A semen sample can show blood and signs of infection


Causes & Risk Factors
Bacterial prostatitis is caused by a bacterial infection that usually occurs when bacteria travel from the urethra into the prostate. In most cases, bacteria in your urine leak into your prostate and cause an infection. With chronic bacterial prostatitis, bacteria chronically infects the prostate gland, leading to repeated urinary tract infections.
The cause of chronic pelvic pain varies. It can come from an initial infection of the prostate, an injury, surgery involving the prostate or lower urinary tract, and spasms of the pelvic floor muscles.
A 2016 study published in Prostate Cancer and Prostatic Diseases by Chen X et al titled “Association of diet and lifestyle with chronic prostatitis/chronic pelvic pain syndrome and pain severity: a case-control study”, indicates potential risk factors for chronic prostatitis/chronic pelvic pain. The most common risk factors include stress, smoking, alcohol consumption, minimal water intake, imbalanced diet, frequent sexual activity, delaying ejaculation, holding urine and nightshift work. Living a sedentary life, drinking caffeinated drinks and not drinking enough water were found to be associated with severe pain in patients with prostatitis.
Some other risk factors associated with prostatitis include having an infection in the bladder that spreads to the prostate; having pelvic trauma; having a prostate biopsy; or having a catheter inserted into the urethra to drain your bladder.
Conventional Treatment
Treatment for acute and chronic bacterial prostatitis typically includes antibiotics and pain relievers. For acute bacterial prostatitis, taking antibiotic medicine for one to two weeks is the most common form of treatment. For some patients with acute bacterial prostatitis, high doses of intravenous antibiotics are necessary because the symptoms come on suddenly and they can be severe. But patients who are not vomiting and aren't seriously ill are usually given oral antibiotics, like fluoroquinolone.
Murphy AB et al 2009 research conducted at Northwestern University Feinberg School of Medicine in Chicago indicates that fluoroquinolone provides relief in 50 percent of men and is more effective when prescribed soon after symptoms begin. The research was published in the journal Drugs titled “Chronic prostatitis: management strategies”.
Most patients with chronic bacterial prostatitis are given low-dose antibiotics for a longer period of time, usually four to six weeks, but treatment can be longer if there aren't results, says J. Curtis Nickel(2011) published in the Canadian Urological Association Journal titled “Prostatitis”
Alpha-blocking agents like tamsulosin and alfusozin are sometimes used to reduce abnormal urinary symptoms in men with prostatitis. These medications are used to help men who experience pain and discomfort when urinating; do not empty their bladders completely; or have trouble urinating.
J. Curtis Nickel and Naji Touma (2012) research published in the Reviews in Urology titled “α-Blockers for the Treatment of Chronic Prostatitis/Chronic Pelvic Pain Syndrome: An Update on Current Clinical Evidence”, shows that alpha blockers are modestly beneficial in some patients with prostatitis; however, there are several side effects to be aware of when taking alpha blockers , including dizziness, headache, vertigo, chest pain, headache, blurred vision and sleepiness
According to my.clevelandclinic.org, Drugs that relax the muscles of the prostate and bladder are also used to improve or reduce symptoms. Medications that are commonly prescribed include finasteride, doxazosin and terazosin.
Natural Urological Ways to Relieve Prostatitis Symptoms
1. Take Quercetin

Quercetin is a type of flavonoid antioxidant that helps to reduce inflammation and pain associated with nonbacterial prostatitis.
Shoskes DA , Nickel JC (2011) research suggests that quercetin can be helpful for men with bladder or prostate symptoms and pelvic floor pain or spasms. The study titled “Quercetin for chronic prostatitis/chronic pelvic pain syndrome” was published in the Urol Clin North America
In one study by Alain Jean Duclos et al 2007 titled “Current treatment options in the management of chronic prostatitis” published in the Therapeutics Clinical Risk Manag ement, 500 milligrams of quercetin was administered twice a day for four weeks. Patients with chronic prostatitis showed significant improvement and reduced inflammation over the placebo group.
2. Bee Pollen

Studies show that bee pollen may be effective in prostatic conditions because of its anti-inflammatory, analgesic and anti-androgen effects. In fact, the efficacy of bee pollen has been compared to anti-inflammatory drugs like naproxen and indomethacin. According to research by
Vassev et al 2015 titled “Bee Pollen: Chemical Composition and Therapeutic Application”published in Evidence-Based Complementary and Alternative Medicine, “clinicians confirm that, in nonbacterial prostate inflammations, pollen improves the condition of patients by effectively removing the pain.”
The most common way to use bee pollen is to mix ground pollen with foods, like cottage cheese, yogurt, juices or smoothies. To reduce inflammation and boost your prostate health, I suggest taking 1 teaspoon of ground pollen three times a day.
3. Saw Palmetto
One of the most well-known saw palmetto benefits is its ability to improve prostate health and urinary dysfunction in a natural way. According to the research, saw palmetto can actually bind to receptors in the lower urinary tract, thereby improving urinary symptoms of prostatitis like overactive bladder and BPH symptoms. Suzuki et al 2009 research titled “Pharmacological effects of saw palmetto extract in the lower urinary tract” published in the journal Acta Pharmacology Sin ica indicate that it has no known drug interactions and doesn't cause any adverse side effects.
Saw palmetto capsules can be found in most health food stores. Make sure the product label indicates that the contents are standardized and contain 85 to 95 percent fatty acids and sterols.
4. Avoid Inflammatory Foods
To relieve prostatitis symptoms, avoid trigger and inflammatory foods like refined carbohydrates , gluten, sugar and artificial sweeteners, spicy foods, acidic foods, alcohol and too much caffeine. These foods, according to a 2016 study published in Prostate Cancer and Prostatic Diseases by Chen X et al titled “Association of diet and lifestyle with chronic prostatitis/chronic pelvic pain syndrome and pain severity: a case-control study”, and other trigger foods that cause allergic reactions, lead to inflammation in the body and can contribute to pain in the pelvic and lower abdominal areas.
Sometimes it's not the typical inflammatory foods that are leading to prostatitis symptoms, but food allergies or intolerances that cause inflammation and pain. An elimination diet involves removing common allergens from your diet, including gluten, dairy, soy, refined sugars, peanuts, corn, alcohol, eggs and packaged or processed foods. After about six weeks of avoiding these foods, your symptoms may begin to dissipate. If that's the case, then you know that one of these foods is the culprit. One by one, begin adding these foods back into your diet and pay close attention to how your body reacts — this will help you to pinpoint what specific food is causing the problem.
5. Eat Healing Foods
Eating a balanced diet is one of the cornerstones of prostatitis treatment. This means consuming whole and natural foods that help to reduce inflammation, heal your gut and boost your immune system . Consume the following foods regularly:
- vegetables, especially leafy greens and cruciferous vegetables
- fruits, especially berries
- high-fiber foods, like beans, legumes, squash, berries, pears, nuts and seeds
- organic, good-quality protein, like grass-fed beef and wild-caught salmon
- omega-3 foods, including wild-caught fish, walnuts, flaxseeds and chia seeds
- healthy fats, like avocados, coconut oil, olive oil and grass-fed butter
- foods high in zinc, like pumpkin seeds, organic lamb, yogurt, kefir, mushrooms and cashews
- probiotic foods, such as coconut kefir, cultured vegetables and kombucha
It's also important to work on reducing stress and getting enough sleep every night — at least seven hours, as these are risk factors for prostatitis.
6. Try Biofeedback Therapy
Biofeedback therapy is a type of training that teaches patients to control involuntary physiological processes, helping you to relax your muscles and reduce pain. A 2003 study published in the Asian Journal of Andrology found that 60 patients with nonbacterial prostatitis significantly improved their symptoms with biofeedback therapy. Some of the symptoms that were improved include pain or discomfort in the genital, groin and rectal areas. Research by Ye ZQ et al 2003 titled “Biofeedback therapy for chronic pelvic pain syndrome” published in the Asian Journal of Andrology concluded that biofeedback therapy is a safe and effective therapy for chronic pelvic pain.
7. Pelvic Floor Training
Research by Siegel AL 2014 titled by “Pelvic floor muscle training in males: practical applications” published in the journal Urology conducted at the Hackensack University Medical Center in New Jersey indicates that pelvic floor muscle training can help to improve a variety of clinical circumstances impacting men, including pelvic pain , urinary incontinence, overactive bladder, dribbling after urinating, erectile dysfunction and ejaculation issues.
Men with chronic pelvic pain syndrome can practice kegel exercises to relieve their symptoms. First, identify your pelvic floor muscles by stopping urination in midstream — the muscles used to do that are your pelvic floor muscles. To do a kegel, tighten the pelvic floor muscles and hold the contraction for five seconds, then relax for five seconds. Keep repeating this method and as you increase your pelvic floor strength, hold the muscle contractions for longer. To make an impact, you'll have to do kegels everyday, so make it a daily practice, doing about three sets of kegels, at 10 reps per set.
8. Use Essential Oils
The three essential oils that I recommend you use to relieve symptoms are frankincense, myrrh and oregano. Frankincense helps to reduce pain and inflammation, two major issues associated with both bacterial and non-bacterial prostatitis. Myrrh oil has antibacterial properties and it can be used to relax your muscles, helping to ease pain. Both frankincense and myrrh oils can be applied topically to the area right below the genitals twice daily. This was contained in a research conducted by Shulan Su et al 2015 titled “Frankincense and myrrh suppress inflammation via regulation of the metabolic profiling and the MAPK signaling pathway” published in the Reports.
Another report by Yap et al 2014 published in the journal Open Microbiology titled “Essential Oils, A New Horizon in Combating Bacterial Antibiotic Resistance” proved that Oregano essential oil has antibacterial, anti-fungal and antiviral properties and are superior to those of prescription antibiotics because it can effectively kill bacteria without the harmful side effects (like destroying food bacteria in the gut) and risk of antibiotic resistance.
To use oregano oil to treat bacterial prostatitis, combine 3–4 drops with ½ teaspoon coconut oil and take it internally twice daily for a maximum of two weeks.
How is prostatitis diagnosed?
A health care provider diagnoses prostatitis based on
- a personal and family medical history
- a physical exam
- medical tests
A health care provider may have to rule out other conditions that cause similar signs and symptoms before diagnosing prostatitis.
Personal and Family Medical History
Taking a personal and family medical history is one of the first things a health care provider may do to help diagnose prostatitis.
Physical Exam
A physical exam may help diagnose prostatitis. During a physical exam, a health care provider usually
- examines a patient’s body, which can include checking for
- discharge from the urethra
- enlarged or tender lymph nodes in the groin
- a swollen or tender scrotum
- performs a digital rectal exam
A digital rectal exam, or rectal exam, is a physical exam of the prostate. To perform the exam, the health care provider asks the man to bend over a table or lie on his side while holding his knees close to his chest. The health care provider slides a gloved, lubricated finger into the rectum and feels the part of the prostate that lies next to the rectum. The man may feel slight, brief discomfort during the rectal exam. A health care provider usually performs a rectal exam during an office visit, and the man does not need anesthesia. The exam helps the health care provider see if the prostate is enlarged or tender or has any abnormalities that require more testing.
Many health care providers perform a rectal exam as part of a routine physical exam for men age 40 or older, whether or not they have urinary problems.

Medical Tests
A health care provider may refer men to a urologist—a doctor who specializes in the urinary tract and male reproductive system. An urologist uses medical tests to help diagnose lower urinary tract problems related to prostatitis and recommend treatment. Medical tests may include
- urinalysis
- blood tests
- urodynamic tests
- cystoscopy
- transrectal ultrasound
- biopsy
- semen analysis
Urinalysis. Urinalysis involves testing a urine sample. The patient collects a urine sample in a special container in a health care provider's office or a commercial facility. A health care provider tests the sample during an office visit or sends it to a lab for analysis. For the test, a nurse or technician places a strip of chemically treated paper, called a dipstick, into the urine. Patches on the dipstick change color to indicate signs of infection in urine.
The health care provider can diagnose the bacterial forms of prostatitis by examining the urine sample with a microscope. The health care provider may also send the sample to a lab to perform a culture. In a urine culture, a lab technician places some of the urine sample in a tube or dish with a substance that encourages any bacteria present to grow; once the bacteria have multiplied, a technician can identify them.
Blood tests. Blood tests involve a health care provider drawing blood during an office visit or in a commercial facility and sending the sample to a lab for analysis. Blood tests can show signs of infection and other prostate problems, such as prostate cancer.
Urodynamic tests . Urodynamic tests include a variety of procedures that look at how well the bladder and urethra store and release urine. A health care provider performs urodynamic tests during an office visit or in an outpatient center or a hospital. Some urodynamic tests do not require anesthesia; others may require local anesthesia. Most urodynamic tests focus on the bladder's ability to hold urine and empty steadily and completely and may include the following:
- uroflowmetry, which measures how rapidly the bladder releases urine
- postvoid residual measurement, which evaluates how much urine remains in the bladder after urination
Cystoscopy . Cystoscopy is a procedure that uses a tubelike instrument, called a cystoscope, to look inside the urethra and bladder. An urologist inserts the cystoscope through the opening at the tip of the penis and into the lower urinary tract. He or she performs cystoscopy during an office visit or in an outpatient center or a hospital. He or she will give the patient local anesthesia. In some cases, the patient may require sedation and regional or general anesthesia. An urologist may use cystoscopy to look for narrowing, blockage, or stones in the urinary tract.
Transrectal ultrasound . Transrectal ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. The health care provider can move the transducer to different angles to make it possible to examine different organs. A specially trained technician performs the procedure in a health care provider's office, an outpatient center, or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images; the patient does not require anesthesia. Urologists most often use transrectal ultrasound to examine the prostate. In a transrectal ultrasound, the technician inserts a transducer slightly larger than a pen into the man's rectum next to the prostate. The ultrasound image shows the size of the prostate and any abnormalities, such as tumors. Transrectal ultrasound cannot reliably diagnose prostate cancer.
Biopsy. Biopsy is a procedure that involves taking a small piece of prostate tissue for examination with a microscope. An urologist performs the biopsy in an outpatient center or a hospital. He or she will give the patient light sedation and local anesthetic; however, in some cases, the patient will require general anesthesia. The urologist uses imaging techniques such as ultrasound, a computerized tomography scan, or magnetic resonance imaging to guide the biopsy needle into the prostate. A pathologist—a doctor who specializes in examining tissues to diagnose diseases—examines the prostate tissue in a lab. The test can show whether prostate cancer is present.
Semen analysis. Semen analysis is a test to measure the amount and quality of a man's semen and sperm. The man collects a semen sample in a special container at home, a health care provider's office, or a commercial facility. A health care provider analyzes the sample during an office visit or sends it to a lab for analysis. A semen sample can show blood and signs of infection
Precautions
A proper treatment plan depends on the cause of the condition. Most times, using several forms of therapy at once is most effective. If you plan on using these natural remedies to relieve your symptoms, do it under the guidance of your health care provider. This is especially important if you plan to use oregano oil instead of antibiotic medications for bacterial prostatitis, as the symptoms come on quickly and can be extremely severe when the condition isn't treated immediately. If you do use antibiotic drugs for treatment, follow it up with a probiotic supplement and probiotic foods in order to replenish the healthy bacteria in your gut.
Combination Natural Therapies together is the best!
One Product designed also for prostatitis is Men's Formula. It is a *research-based*, *scientific*, ingredients of *14 herbs*for prostate health* and *an immune booster to improve the quality of life of men with advanced prostate problems*. The special formulation of over fourteen (14) herbs, all *synergistically* balanced to support the *male reproductive* and *urinary systems*-particularly the *prostate and kidneys*, *assisting the prostate in cellular regeneration* for ultimate health and well-being*.
*The extracts are: Hibiscus Sabdarrifa, Azadirachta indica, carica papaya,Graviola, stinging Nettle, Zanthoxyllum zanthoxyloides, small willow herb, saw palmetto, pumpkinseeds,cyperus esculentus, Altsonia Boonei, Africa black pepper, Allium Sativum, Zingiber Officinale and many more blended together. *
Final Thoughts
- The term prostatitis describes a combination of infectious diseases that involve the prostate gland. In a nutshell, it's a common condition that involves an infection or inflammation of the prostate.
- The four types are acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome and asymptomatic inflammatory prostatitis.
- The most common symptoms are pain during urination; trouble urinating; frequent urination; pelvic pain, lower back pain, and pain in the genital or groin areas.
- Prostatitis is caused by bacteria that usually travel from the urine, through the urethra and into the prostate; trauma to the prostate or lower urinary tract; or spasms of the pelvic floor muscles.
- The best natural ways to relieve symptoms include quercetin, bee pollen, saw palmetto, eliminating trigger foods, eating a healing diet, trying biofeedback therapy, practicing pelvic floor muscle training and using essential oils, especially frankincense, myrrh and oregano.
- Men's Formula product is an all-natural therapy formulator also to support the prostate and immune health to treat prostatitis. Formulated with over 14 plants. It can be combined with other products to aid faster treatment.
About the author: Dr. Raphael Nyarkotey Obu, is an honorary Professor of Naturopathic Medicine with research interest in Holistic Urology, prostate cancer in black men, prostate health, Natural Men's Health-Vinnytsia State Pedagogical University, Ukraine, President of Nyarkotey College of Holistic Medicine, Tema Community, 7, Post Office. Formulator of Men's Formula for Prostate Health & Immune booster, Women's Formula for wellness and Nyarkotey Tea for Cardiovascular Health. Enquiries: 0208244716/0541234556, Kumasi: 0243611641
References:
1] Nickel JC. Prostatitis and related conditions, orchitis, and epididymitis. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 10th ed. Philadelphia: Saunders; 2012: 327–356.
[2] Barry MJ, Collins MM. Benign prostatic hyperplasia and prostatitis. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine. 24th ed. Philadelphia: Saunders; 2011: 805–810.
[3] Murphy AB, Macejko A, Taylor A, Nadler RB. Chronic prostatitis: management strategies. Drugs. 2009;69(1):71–84.




 E-Cedi will be used as a weapon to fight money laundering and corruption — Bawum...
E-Cedi will be used as a weapon to fight money laundering and corruption — Bawum...
 Election 20204: Transfer power to us peacefully for your own good — NDC tells NP...
Election 20204: Transfer power to us peacefully for your own good — NDC tells NP...
 Voter registration: Don't bus minors to registration centres — Nana Akomea warn ...
Voter registration: Don't bus minors to registration centres — Nana Akomea warn ...
 Error in registration slip: Trust the Commission on its mandate — EC assure Ghan...
Error in registration slip: Trust the Commission on its mandate — EC assure Ghan...
 Ejisu by-election: NPP aspirant who projected less than 5% votes for Aduomi cong...
Ejisu by-election: NPP aspirant who projected less than 5% votes for Aduomi cong...
 Election 2024: Stolen BVR kits could be used to illegally register people – NDC ...
Election 2024: Stolen BVR kits could be used to illegally register people – NDC ...
 60% of SHSs taken off double track system – Dr Yaw Osei Adutwum
60% of SHSs taken off double track system – Dr Yaw Osei Adutwum
 Voter registration: We hope to hit over one million registered voters in Volta -...
Voter registration: We hope to hit over one million registered voters in Volta -...
 Akufo-Addo not obliged to disclose full KPMG audit report – Presidency
Akufo-Addo not obliged to disclose full KPMG audit report – Presidency
 ECG staff used ransomware to sabotage paperless system, can you imagine they eve...
ECG staff used ransomware to sabotage paperless system, can you imagine they eve...
