FUNGAL SKIN INFECTIONS
20-25% of the world's population has fungal skin infections.
Fungal skin infections caused by fungi that thrive on skin keratin (dermatophytes), are from the genera: Microsporum (M), Epidermophyton(E) and Trichophyton(T). Infections caused by these fungi are called Tinea (ringworm).
Yeasts, including Candida, and Malassezia species, (both of which are normal skin commensals), are other fungi that cause skin infections.
FACTORS PROMOTING FUNGAL SKIN INFECTION.
. Warm and humid weather conditions favor fungal growth on the skin.
. Zinc deficiency: Zinc is an important nutrient required for normal skin function
Zinc, together with vitamin D and selenium, help the body (liver and kidneys) to produce metallothioneins.
Metallothioneins are proteins that naturally kill fungi.
Zinc deficiency promotes the growth of candida on the skin and vagina.
Food high in phytic acid like maize and beans may promote fungal skin growth. (Phytic acid binds zinc in the intestines and are excreted in waste.) Zinc supplements are necessary to prevent zinc deficiency and fungal growth.
Other factors that promote fungal skin infections include:
. Sweating a lot
. Using public showers and bathrooms
. Wearing damp innerwear and socks
. Recent antibiotics use.
. Being overweight, Diabetic or taking steroids.
. Previous fungal skin infection.
. Those with weakened immunity like HIV,
. Contacts with house pets like cats, and rodents like rats, guinea pigs, and mice
. Walking barefoot
A.) TINEA/RING WORM
Tinea refers to fungal infection of skin keratin. Tinea infections are common in children. In prepubertal children, tinea capitis and tinea corporis are most common. In adolescence and adults, tinea pedis, tinea cruris, and tinea unguium are common.
Tinea are categorized according to the area of the body involved.
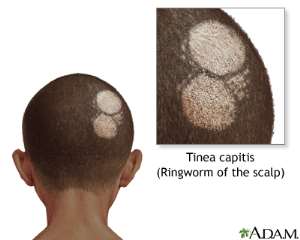
1.) RINGWORM OF THE SCALP /TINEA CAPITIS
Tinea capitis is caused by fungi of Trichophyton and Microsorum species.
In UK and North America, T. tonsurans causes majority of tinea capitis. Microsporum species common in West Africa.
Source of infection: cats, puppies, cattle
Tinea capitis commonly affects children 3-10 years old, and some adults too, especially in crowded conditions.
Transmission: by indirect contact with fallen hair and epithelial cells, through combs, hair brushes and other barber shop instruments. Co-sleeping has been associated with spread of tinea capitis
One can be infected by this fungus, without developing any symptoms, and become a carrier instead.
Features:
Hair loss and inflammation of the affected scalp area are the hallmarks.
Inflammation may manifest as:
1.Scalp scaling, and greyish patches. If left untreated, there is a risk for developing:
2. Severe inflammation and abscess formation (kerion), which may lead to scarring and permanent baldness
3. Formation of Yellow crusts around hair follicles (favus)
Hair loss manifest as:
1. Black dots: broken hair shaft close to the scalp.
2. Discrete patches of hair loss
Diagnosis: Microsporum infected scalp emit brilliant green flourescence with wood's lamp
Potassium hydroxide preparation
Prevention, Tinea capitis:
Stop sharing towels, combs, hair brushes
Disinfect (or discard) pillows, hats, combs, scissors if a family member has the infection
Wash bed linen and clothes to get rid of fungal spores.
Household Cats and dogs must be examined under wood's lamp and referred to veterinary service for therapy.
Treating all asymptomatic household contacts, including adults may be beneficial.
TREATMENT OF TINEA CAPITIS:
Systemic antifungals using:
Griseofulvin 20mg/kg/day for 6 weeks or
Terbenafine 5mg/kg/day for 4 weeks.
The child may attend school, once they are started on oral medications.
2.) ATHLETE'S FOOT (TINEA PEDIS) & ONYCHOMYCOSIS
Athlete's foot infections commonly occur in between the toes, but may occur in other areas of the feet, including the sides and soles, and even on the hands.
Etiology: Trichophyton rubrum, (worldwide) E. Floccosum and T tonsurans
Infection occurs with direct contact with contaminated skin, left behind in public showers, bathrooms and swimming pool.
The fungus grows best under dark, damp and warm conditions such as shoes.
Symptoms include:
Flaky whitish scales, involving the plantar surfaces and along the sides of the feet,
Scaly red or whitish, itchy areas between the toes, leading to maceration and fissuring.
The same agents cause toenails infection, which affects one in ten adults.
ONYCHOMYCOSIS
With tinea unguium (ring worm infection of nails), the condition starts as yellow spot under the tip the nails. As infection goes deeper, the nails become thickened, malformed, discolored with brittle with crumbling edges.
Complications:
. May become painful, and may interfere with activities
. Toenail disfigurement may lead to loss of self-esteem and inhibited social interactions.
Risk factors for toenail infections:
. Persons with Poor circulation.
. Persons with diabetes
. People with hyperhydrosis pedis (sweaty feet).
Diagnosis is carried out by dissolving the debris under the nail in 20% potassium hydroxide and examining for hyphae under light microscope.
Prevention
Wear plastic shoes in communal areas such as swimming pools, change rooms
Don't wear the same shoes every day. Allow the shoes to dry out. Alternate shoes, every other day.
Wear cotton socks, and antifungal drying powder, when wearing shoes.
Old shoes may act as sources of reinfection. Treat with antifungal powder or throw them away.
Scrub your feet and toe web spaces, regularly, to dislodge contaminated debris.
Avoid walking barefoot
TREATMENT
a.) Athlete's feet: Topical antifungals:
Miconazole2% lotion,
Clotrimazole 1%,
ketoconazole,
Terbinafine1%. (Nystatin not effective)
b.) Onychomycosis, a combination of oral antifungal and topical antifungals improve the cure rate. Terbinafine and Itraconazole penetrate the nail plates within a few days of initiating treatment.
Terbinafine 250mg daily for 12 weeks (6 weeks for fingernail). Avoid terbinafine in persons with liver diseases
Itraconazole 200mg/day for 12 weeks
3.) TINEA CORPORIS, & TINEA CRURIS
Ringworm is a name used to describe a type of itchy ring-like rash (red annular rash with scaly edges and normal skin in the center).
Tinea cruris (jock itch) is a Ringworm of the groin, inner thigh, and buttocks. It does not involve the scrotum. (It is candida intertrigo, that involves the scrotum). Infection result from seeding the fungi (scratching) the groin, after scratching an infected athlete foot
Tinea corporis is ringworm of the rest of the body (scalp, groin, palm and feet excluded). It often involves exposed areas of the body, such as abdomen, limbs. The rashes may coalesce to form larger rash, as they expand from the center.
Diagnosis: Potassium hydroxide examination of skin scrapings.
PREVENTION OF TINEA CORPORIS
Wear lose fitting clothes and underwear
Wear cotton socks and cotton or natural fiber underwear to allow the skin to breathe
TREATMENT:
Topical Antigungals:
Naftifine 1% cream,
Terbinafine cream
B.) THE YEAST SKIN INFECTIONS
The yeast infections include pityriasis versicolor, and intertrigo
PITYRIASIS/TINEA VESICOLOR
Vesicolor means various colors. Tinea versicolor is very common in the tropics.
Malassezia species are normal skin yeast that flourishes and may overgrow to cause skin infection under wet skin conditions related to sweat, warm and humid weather, and in the presence of zinc deficiency.
Skin infections result with the formation of either: hypopigmented and or hyperpigmented patches that are dry and a bit scaly on the skin.
The condition can become chronic and last for many years. The rash may be on the upper back, abdomen, neck, limbs.
In the Preadolescence: facial involvement is common.
Diagnosis:
Under wood's light, the lesions appear chamois leather-like (pale yellowish to white)
When skin scrapings are prepared with potassium hydroxide and examined under microscope the fungi appear as grapelike clusters of spores on short hyphae, giving the appearance of spaghetti and meatball
PREVENTION OF TINEA VERSICOLOR:
Cotton clothing may help keep moisture away from the skin
Dry your skin carefully after bathing
Wear synthetic fibers that wick the sweat away from the body, helping keep the skin dry, if one is exercising.
TREATMENT OF PITYRIASIS VERSICOLOR:
Topical antifungals:
Selenium sulfide 2.5% shampoo or lotion, apply daily for 10-15 minutes, prior to rinsing; for 2 weeks
Ketoconazole 2 % shampoo 10 minutes (before washing it off) daily for 5 days,
Once monthly application of these topical agents, help to prevent rcurrences.
Systemic antifungals:
Ketoconazole 400mg oral x1 dose (not FDA approved, and is less effective than prolonged use of topical agents)
INTERTRIGO
Intertriginous inflammation of the skin is not a primary fungal disease. It is rather an opportunistic fungal infection. The primary problem is skin folds inflammation resulting from a combination of skin friction, heat, moisture, poor ventilation. This provides fertile ground for candida albicans to infect such areas.
It usually occurs in warm and humid environmental conditions.
Skin areas such as:
. Armpits,
. the skin under large breasts,
. In the groin including the vulva and scrotum
. Between the buttocks
. Neck creases
. fat folds on the abdomen are, usually involved.
There may be red or brown-red rash; raw, itchy, or oozing skin with Foul odor. The skin may be cracked or crusty.
Affected persons may complain of itching, burning, pain and intermittent stinging at affected areas.
Supra-infection with skin bacteria may occur
DIAGNOSIS
Potassium hydroxide examination of scrapings under microscope, shows pseudo-hyphae ad spores
Prevention
Weight loss if overweight
Wear brazier with good support
Keep skin dry and as cool as possible.
Reducing skin friction and moisture with barrier paste and Zinc oxide powder are important in intertrigo prevention.
TREATMENT
Primary intertrigo may be treated with topical drying agents
Topical gel: fluconazole, or itraconazole, plus low potency topical steroids/




 Minority will expose the beneficial owners of SML, recover funds paid to company...
Minority will expose the beneficial owners of SML, recover funds paid to company...
 Prof. Opoku-Agyemang has ‘decapitated’ the NPP’s strategies; don’t take them ser...
Prof. Opoku-Agyemang has ‘decapitated’ the NPP’s strategies; don’t take them ser...
 Abubakar Tahiru: Ghanaian environmental activist sets world record by hugging 1,...
Abubakar Tahiru: Ghanaian environmental activist sets world record by hugging 1,...
 Prof. Naana Opoku-Agyemang will serve you with dignity, courage, and integrity a...
Prof. Naana Opoku-Agyemang will serve you with dignity, courage, and integrity a...
 Rectify salary anomalies to reduce tension and possible strike action in public ...
Rectify salary anomalies to reduce tension and possible strike action in public ...
 Stop all projects and fix ‘dumsor’ — Professor Charles Marfo to Akufo-Addo
Stop all projects and fix ‘dumsor’ — Professor Charles Marfo to Akufo-Addo
 Blue and white painted schools will attract dirt shortly – Kofi Asare
Blue and white painted schools will attract dirt shortly – Kofi Asare
 I endorse cost-sharing for free SHS, we should prioritise to know who can pay - ...
I endorse cost-sharing for free SHS, we should prioritise to know who can pay - ...
 See the four arsonists who petrol-bombed Labone-based CMG
See the four arsonists who petrol-bombed Labone-based CMG
 Mahama coming back because Akufo-Addo has failed, he hasn't performed more than ...
Mahama coming back because Akufo-Addo has failed, he hasn't performed more than ...
