Sex workers are one of the most vulnerable social groups in the world. They experience widespread stigma, discrimination, state and non-state violence and harassment. This results in decreased access to services – including healthcare.
This is a serious problem for female sex workers who have frequent sexual contact with multiple partners which puts them at risk of acquiring HIV and other sexually transmitted infections. Other risks include unwanted pregnancies, induced abortion, sexual violence and cervical cancer.
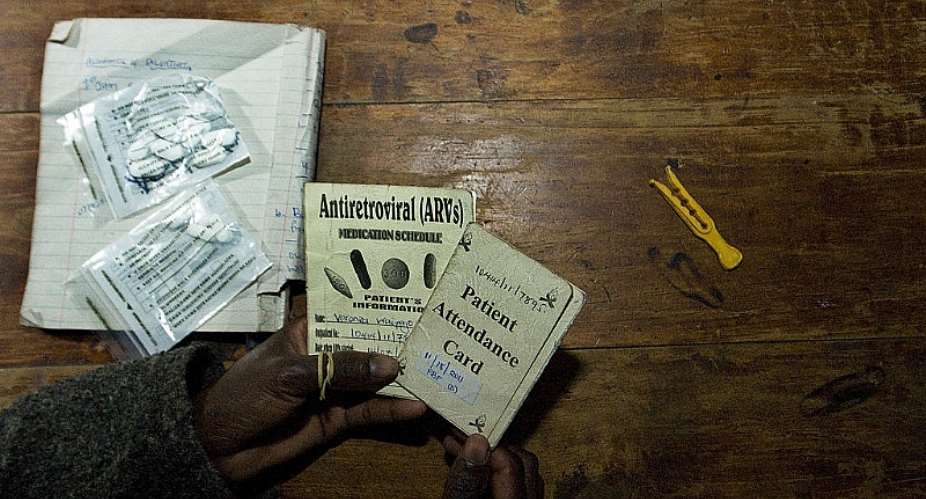
HIV and sexual and reproductive healthcare, in particular, are critical for female sex workers. Many who are living with HIV rely on antiretroviral (ARV) medication for good health. Any disruptions to access would have serious consequences. Estimates show that a disruption in the supply of ARVs lasting six months could lead to over 500,000 HIV-related deaths among adults in sub-Saharan Africa.
Unfortunately, COVID-19 has made it even harder for sex workers all over Africa to access healthcare.
In Kenya, to control the spread of the new coronavirus, the government enacted strategies to manage the disease which created major challenges for various groups of society, including female sex workers. These included movement restrictions, dusk to dawn curfews, social distancing measures and the closure of bars and nightclubs.
We wanted to know how the government's strategies had impacted female sex workers and their ability to access healthcare in Nairobi, the country's capital. There are at least 20,000 sex workers in Nairobi, most of whom are women. Kenya does not criminalise sex work, but there are a number of other laws which can be used to oppress sex workers.
We found that the COVID-19 restrictions created life-threatening challenges to female sex workers as they weren't able to access their medication, support or their clients.
Sex workers are a marginalised and vulnerable group of women and young girls, with no recourse to public protection. This means the burden falls on NGOs to ensure healthcare is available and accessible.
What sex workers said
We collected data from 117 female sex workers living in informal settlements in Nairobi. We also collected data from 15 healthcare providers and from workers at the Bar Hostess Empowerment and Support Programme – an organisation that supports sex workers.
Sex workers typically use clubs and bars as a safe a space to meet clients. But, under the restrictions, these were closed or had limited operating hours. This meant that their livelihood was removed overnight. This made medication, as well as transport to visit clinics, a luxury they couldn't always afford.
The restriction of movement in and out of Nairobi was a huge challenge for many. It was introduced abruptly leaving no consideration for those who had temporarily travelled out of Nairobi to go back to their homes. Some sex workers in our study were stranded outside the city without knowledge of alternative services which could meet their healthcare needs. One sex worker said:
I am a mobile sex worker (call girl), I had travelled out of town with a client. After the movement ban in and out of Nairobi, the client left to pick up something in Nakuru town leaving me in the hotel room. But he never came back for like two days. I was unable to sustain the bills so I had to be chased out of the hotel. Now I am unable to access the health services that I need, I am still new here in Nakuru and I don't know anyone here it's really a challenge to access any medical service.
Restrictions of movement within the city also meant that some sex workers weren't able to access their usual clinics. As one sex workers described:
I have missed my appointments to the clinic… I was supposed to go collect my ARVs but now with the lockdown, how will I go to collect them? I cannot visit the public health facility because of stigma and discrimination.
Fuelled by the government's restrictions, we also found that sex workers were too afraid to use health services out of fear of contracting COVID-19.
Dusk to dawn curfew
The dusk to dawn curfew was cited as a key barrier to healthcare access for sex workers.
An outreach worker at one of the clinics explains that the curfew denies young sex workers adequate time to interact and share at their “Safe Space”. These spaces are provided by three healthcare centres – run by the Bar Hostess Empowerment and Support Programme across the city and are accessed by hundreds of young people each day – usually for medication and reproductive health services. They also use the space for education, to share their experiences and offer support.
The night curfew also forced the sex workers to change their operations and work during the day. In some cases this meant that sex workers were forfeiting visits to the clinics because they had limited time during the day to work and go to seek healthcare services before the curfew hours.
Curfew restrictions and cessation of movement coupled with police brutality on those found breaking the rules further intensified the challenges of accessing healthcare for sex workers as observed by a health worker:
Recently some clients from Biafra tried to sneak out to come to the drop-in centre for services but the police found them and turned them back. The police are really mistreating them.
A way forward?
There are solutions. The Bar Hostess Empowerment and Support Programme and the University of Leicester, in the UK, invented practical responses to the effects of COVID-19. One of these was to use motorbikes to deliver essential commodities needed by sex workers, with a service user population of 20,000 sex workers. The programme is reaching out to many people each day to provide urgent medication, support and advocacy.
In addition to this, a mobile phone application has been created to enhance access to the clinics and the facilities at Bar Hostess Empowerment and Support Programme for the service users. This will cushion sex workers during the COVID-19 period and the longer term impacts of this pandemic.
Teela Sanders receives funding from the University of Leicester Global Challenges Research Fund.
Rahma Hassan does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
By Teela Sanders, Professor in Criminology, University of Leicester And
Rahma Hassan, PhD Fellow, University of Nairobi




 We’ll protect state wealth from opaque deals – Prof Jane Naana
We’ll protect state wealth from opaque deals – Prof Jane Naana
 Mauritania president says running for second term in June polls
Mauritania president says running for second term in June polls
 I won't ever say I was a mere driver’s mate' — Prof. Opoku-Agyemang
I won't ever say I was a mere driver’s mate' — Prof. Opoku-Agyemang
 2024 polls: 'EC struggling to defend credibility'— Prof. Opoku-Agyemang
2024 polls: 'EC struggling to defend credibility'— Prof. Opoku-Agyemang
 Akufo-Addo gov't's 'greed, unbridled arrogance, unrestrained impunity, sheer dis...
Akufo-Addo gov't's 'greed, unbridled arrogance, unrestrained impunity, sheer dis...
 Election 2024: Ghana needs an urgent reset, a leadership that is inspiring – Ma...
Election 2024: Ghana needs an urgent reset, a leadership that is inspiring – Ma...
 Partner NDC to rollout a future of limitless prospects – Prof Jane Naana Opoku-A...
Partner NDC to rollout a future of limitless prospects – Prof Jane Naana Opoku-A...
 NPP will remain in gov’t till Jesus comes — Diana Asamoah
NPP will remain in gov’t till Jesus comes — Diana Asamoah
 Sunyani Technical University demands apology from former SRC president over sex-...
Sunyani Technical University demands apology from former SRC president over sex-...
 'Dumsor' was resolved by Mahama but ‘incompetent' Akufo-Addo has destroyed the g...
'Dumsor' was resolved by Mahama but ‘incompetent' Akufo-Addo has destroyed the g...
