Men don’t cry, but today, Ghanaian men are crying and this is what I have realized from my research with Ghanaian men and prostate cancer. My research interest is strictly on how men of West African descent viewed prostate cancer and how prostate cancer affects men of African descent.
This current study is focused on men and women I had encountered with during an invitation I received to provide expert talk on prostate cancer for Aviation staff this year and my daily interaction with Ghanaian men and women on prostate cancer . I am also working on a research paper on men’s Health in context in Ghana with Michelle Williams, PhD, MPH, CHES-University of Alabama at Birmingham as a coauthor of the paper.
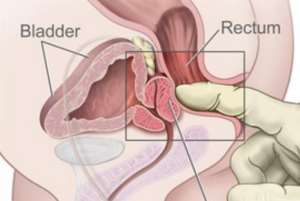
Sex after prostate cancer is a serious issues affecting lot of Ghanaian men diagnosed or yet to undergo conventional prostate cancer treatment. Most Men diagnosed with prostate cancer tried to forgo conventional treatment because of the information they received regarding prostate cancer treatment and their sex life. Men always want to protect their sex life and don’t want to lose it but men in Ghana don’t know why the prostate gland is that powerful and is the bedrock of the men sex life though it is a small gland but with huge repercussions on the quality of life on Ghanaian men.
“I know within me; I am sleeping on duty!
I sometime have to sleep early or pretend to be sick to avoid my wife torching me or demanding to have sex with her; partly because, I can no longer ride the mountain that I used to do. There is always a quarrel in the night when it is time for work. I am unable to have an open communication with my wife to tell her my problem to avoid me losing her to another man.
I am suffering from the side effect of conventional prostate cancer treatment
(A prostate cancer patient’s quote on his experience with sex after prostate cancer treatment)
76% of all men diagnosed with prostate cancer will suffer either permanent or temporal erectile dysfunction and could go on to about 95% after radical prostatectomy-that is surgery to remove the prostate gland and the quality of treatment for prostate cancer men received and survival rates also depends upon where men leave, but do men even get the right treatment for the amount they paid for conventional cancer treatment in Ghana? There are more questions than answers!
Masculinity
“My manhood has shrunk after prostate cancer treatment leaving me thinking”- A patient quote.
Sexual dysfunction is one of the most prevalent and distressing consequences of prostate cancer. Despite this, very little is known about the management of sexual dysfunction and current health care services do not adequately meet sexual health needs of survivors.
Some men find that their penis is shorter after surgery (radical prostatectomy). This happens because of changes to the tissue inside the penis. Other treatment such as hormone therapy with radiotherapy may also cause changes to the size of your penis.
Encouraging blood flow to the penis after surgery may improve erections and stop your penis becoming smaller. In particular, using a vacuum pump on its own or with PDE5 tablets may help maintain your penis size and improve erections. This is called penile rehabilitation.
Effects of prostate cancer treatment
Treatment for prostate cancer can cause a variety of side effects. Any of these can affect your sex life, some more than others. The effects you have will depend on the treatment you have had.
You may not feel like sex at all while you are having your treatment, or for some time after you are diagnosed. Many people feel very low after they have been told they have cancer and don't feel interested in sex. But some people react to their diagnosis by feeling they should be packing as much into life as possible. If you feel like this, and treatment has caused erection problems , this may be hard to bear.
Whatever happens at first, remember that things will change. To see how your sex life will be affected, you will need to wait until at least the end of your treatment. And it is best to wait until you are feeling more back to normal.
Some of the side effects listed here are temporary – for example, tiredness and diarrhoea due to radiotherapy will wear off some weeks after your treatment has finished.
Prostate cancer cannot be pass on to a partner
Some men worry that they may pass on prostate cancer in their semen during sex. This is not true. Cancer is not infectious and cannot be passed on to another person in this way. But this can be a very real anxiety. It is important to understand how powerful this fear can be. Talking it through with a partner and getting reassurance from them can be helpful.
Some people find that they need outside help to discuss this issue. They may benefit from talking to a counsellor, the doctors and nurses at the hospital, or a sex therapist. These people are aware of the difficulties people have with cancer and can offer specialist advice and support.
Diarrhoea
Some men get diarrhoea during radiotherapy and for some time afterwards. This can be unpleasant and tiring and may put you off wanting to have sex. It will gradually go back to normal after a few weeks though.
Tiredness
You may feel too tired to want sex for some time after prostate cancer treatment
Leakage of urine
If you have leakage of urine (incontinence) or a catheter into your bladder, you may feel embarrassed and that may put you off sex.
Less interest in sex
Being less interested in sex can be a side effect of surgery to remove the testicles (orchidectomy) , or hormone treatment . Unfortunately, a lower interest in sex cannot be treated with testosterone injections or patches as it normally would. This is because the testosterone could encourage the cancer to grow or come back.
Lack of interest in sex and erection problems are less likely to occur with anti androgen drugs like bicalutamide , than other types of hormone therapy. So changing your hormone treatment may help. You would need to discuss this with your specialist.
The effects on your sex life can be difficult to live with. The way that the side effects affect you will depend on your own individual situation. It will also depend on your partner (if you have one) and how your sexual relationship has been in the past. It will help to talk things over with your partner and discuss the changes in your lives.
Hot flushes and sweats
Hot flushes and sweats can be a side effect of hormone therapy or removal of the testicles (orchidectomy). They may be at their worst when you have just started your hormone treatment, or have just had your testicles removed. The flushes and sweats may get better with time. They may become less frequent or stop altogether. Or you may not be troubled by them at all.
Everyone reacts to cancer treatment in different ways, both emotionally and physically. If you are having problems with sweats and flushes talk to your doctor or specialist nurse. They can prescribe medicines to help.
Difficulty getting an erection (impotence)
Difficulty in getting an erection can be caused by the following types of treatment.
- Radiotherapy to the prostate
- Prostate surgery
- Having both testicles removed
- Most types of hormone therapy
Erection difficulties can be very difficult to come to terms with. After surgery you are very likely to have erection problems. This may be temporary, but if you have had the prostate gland removed ( radical prostatectomy ), it is more likely to be permanent.
Hormone therapy can also affect your ability to have an erection. If you stop the injections or tablets, the erections may improve.
With radiotherapy , erection problems may start up to 2 years after your treatment because of nerve damage. It can take that long for nerve damage to show up after any radiotherapy.
If you have erection problems, medicines such as sildenafil citrate (Viagra), vardenafil (Levitra) or tardenafil may help. If these treatments are started early they can sometimes help to prevent erection problems developing. Other forms of treatment include gels (MUSE), injections (Caverject) or vacuum devices to give an artificial erection. Alternative remedies are also available
Your erection problems
Erection problems can be permanent or temporary. And they can be affected by your mood and feelings. If you are having problems, they may sometimes be caused by anxiety and not the effects of treatment. You may find it difficult to talk about these both with your doctor and with your partner.
If you are worried about talking to your partner, it may be because you are afraid that they might reject you, or be angry with you in some way. But your partner may be wanting to talk things over.
Infertility and prostate cancer treatment
Treatment for prostate cancer will mean that you cannot father children in the future. This is called infertility. This can be very hard to accept, especially if you were hoping to have children. You and your partner need to discuss this with your doctor before you start treatment, particularly hormone treatment or radiotherapy . Some men may want to collect and store sperm before they start treatment.
After surgery to remove the prostate gland you don't produce semen. If you have had a TURP operation , you will probably have retrograde ejaculation after surgery. Retrograde ejaculation means that when you orgasm, your sperm goes backwards into your bladder, rather than out through your penis. This is because there is a valve that normally shuts off the route to the bladder when you climax, and this is damaged in the TURP operation. In this situation, if you want to have children, it may be possible to take sperm directly from your testicles. The sperm can be used to fertilise your partner directly or with the test tube baby technique (in vitro fertilization or IVF).
Clinical Recommendations
All men define their masculinity as a part of normal development. When they have to restructure that definition due to sexual dysfunction, few will view that restructuring positively. Yet, men need to be reminded that even without ideal erections, much of their sexuality remains. Sexual feelings, penile sensitivity, orgasms and partnered intimacy (in many cases) are available. Helping men recognize sexuality as a much larger concept than erectile function is an important intervention that reframes the prostate cancer-related sexual side effects. Creating an accepting health care environment for men's vulnerability and feelings about the loss of erections will help them approach mourning as the gateway to a new sexual adaptation alone or with a partner. Movement forward is easier when change is acknowledged, understood, grieved and mourned.
In most cases, this may be a brief, supportive intervention in the context of a cancer survivorship program, preferably with the partner present. Inclusion of information about menopause helps couples recognize that both individuals may face sexual challenges in middle age. Support for communication about new intimacy will be helpful. This comprehensive approach is likely to minimize barriers to penile rehabilitation and sexual recovery. When brief psychoeducational interventions are insufficient to improve couples' sexual relationship, long-term issues may be impinging on this adaptation, and more intensive sex therapy may be required.
Clinicians should create an environment that includes language and teaching materials that are inclusive to men from other ethnic groups or cultures and their partners. Health care providers may need to expand their knowledge of sexual practices and sexual beliefs .
Availability of psychoeducation about changes in sexuality, sex therapy and couple therapy as a part of prostate cancer care would reassure patients that there is a support structure aimed at restoring intimacy and sexuality. It may encourage help seeking that has been less than optimal to date.
Patients with prostate cancer, partners and clinicians need a sexuality-focused road map to guide them from diagnosis, through treatment to recovery. The road map should include real-time assessments to guide interventions: psycho-education, grief, coping, creation of new sexual possibilities and referral for individual or couple sex therapy. If the sexual recovery road map includes periodic evaluation of its efficacy and effectiveness, it can be successfully integrated into evidence-based treatment of prostate cancer.
Prostate cancer is really a test of Manhood for both Ghanaian men and women. The focus should also be channeled to educate the women to understand the side effect of the disease on their men sex life so that they exercise patience. Sex is not the only way to make a woman happy and the women should understand this fact.
Dr. Raphael Nyarkotey Obu is a registered alternative medical practitioner who specializes in Prostate cancer and studied the Masters program in prostate cancer –Sheffield Hallam University, UK and a PhD candidate in prostate cancer, Indian Board of Alternative Medicines Academy, Kolkata, India and the founder of Men’s Health Foundation Ghana and De Men’s clinic and Prostate Research Lab in Dodowa, Akoto House. Tel: 0500106570




 Akufo-Addo commissions Phase II of Kaleo solar power plant
Akufo-Addo commissions Phase II of Kaleo solar power plant
 NDC panics over Bawumia’s visit to Pope Francis
NDC panics over Bawumia’s visit to Pope Francis
 EC blasts Mahama over “false” claims on recruitment of Returning Officers
EC blasts Mahama over “false” claims on recruitment of Returning Officers
 Lands Minister gives ultimatum to Future Global Resources to revamp Prestea/Bogo...
Lands Minister gives ultimatum to Future Global Resources to revamp Prestea/Bogo...
 Wa Naa appeals to Akufo-Addo to audit state lands in Wa
Wa Naa appeals to Akufo-Addo to audit state lands in Wa
 Prof Opoku-Agyemang misunderstood Bawumia’s ‘driver mate’ analogy – Miracles Abo...
Prof Opoku-Agyemang misunderstood Bawumia’s ‘driver mate’ analogy – Miracles Abo...
 EU confident Ghana will not sign Anti-LGBTQI Bill
EU confident Ghana will not sign Anti-LGBTQI Bill
 Suspend implementation of Planting for Food and Jobs for 2024 - Stakeholders
Suspend implementation of Planting for Food and Jobs for 2024 - Stakeholders
 Tema West Municipal Assembly gets Ghana's First Female Aircraft Marshaller as ne...
Tema West Municipal Assembly gets Ghana's First Female Aircraft Marshaller as ne...
 Dumsor is affecting us double, release timetable – Disability Federation to ECG
Dumsor is affecting us double, release timetable – Disability Federation to ECG
