As a young enthusiastic alternative medical practitioner, in my prostate cancer journey and profession as a registered Naturopathic integrative oncologist, research, prostate cancer policy maker for Men's Health Foundation Ghana and prostate cancer community champion, my research focus on black men and cancer of the prostate cancer specifically men of West African descent and coupled with my learning periods in the first ever master's program in prostate cancer introduced by Sheffield Hallam University, UK and Prostate Cancer UK I have come to realized that, there are lot of rigid dogmas and erroneous statement people make in the subject of prostate cancer. I want men of West African descent to be clear that male menopause does not cause prostate cancer and it is garbage to make such erroneous statement. If it is menopause then, the Okinawans or centenarians are in big trouble!
While there is some uncertainty about male menopause there is no question that age-related changes in men impact testosterone level. Male menopause, or andropause, symptoms occur much more slowly than menopause symptoms in women. Around age 35 or 40, a man's testosterone level naturally begins to decline at a rate of about 1-2% per year, making the term "pause" not entirely accurate. Normal testosterone level, at any age, is measured in a range of 300 to 1,200 nanograms per deciliter. Testosterone is widely accepted as a prostate cancer fuel, and is regularly countered through androgen deprivation therapy for prostate cancer.
If one believes that high T is worrisome for prostate cancer, and then it should follow that low testosterone would be protective against the development of prostate cancer but is this correct? It is also believed that black men have high T level and is one of the factors predisposing them to prostate cancer. There are lots of erroneous statements when it comes to the subject of prostate cancer in the medical community.
Notwithstanding multiple efforts to show that higher T levels lead to an increased risk of cancer of the prostate in black men, there remains no compelling scientific evidence to support this theory. There is an established fallacy coming from the medical institution when it comes to the subject of testosterone and prostate cancer.
It has been thought that testosterone was actually responsible for prostate cancer growth and might possibly cause slow-growing cells to grow more quickly.
So for years, the medical occupation well-educated that by giving testosterone to a man that had been diagnosed with prostate cancer, they were basically 'adding fuel to the fire'.
This was one of the factors that were accountable in leading to numerous men enduring hormone therapy treatments because there was an emphasized link between testosterone and prostate cancer.
The whole idea was that cancer of the prostate needed testosterone to grow and therefore, endorsing hormone therapy treatments is unique in decreasing the testosterone and would therefore stalls the progress and spread of the cancer. So what actually drew my attention to this very controversial subject, very simple, as I was going through my television channels and I came across this discussion on prostate diseases and the doctor made a comment that all men will get enlarged prostate and he also link prostate cancer to menopause in men and I laugh but it was a nice argument anyway. I said to myself this is garbage! Go to Asia countries or do your research well before you appear on television.
You see, it is believed that over 90% of all prostatic diseases would be prevented during the life of all dogs if the animal was castrated in the first year of life. Castration will have no effect on the incidence of cancer, but remember this is very uncommon. Dogs are the only animal we know developed prostate conditions also. You know why? Because dogs also feed on the junk table foods you exposed yourself too!
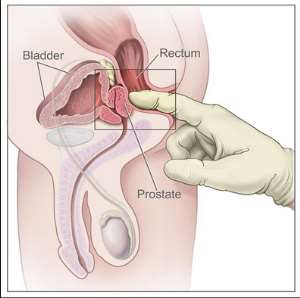
It is also believed that Dogs that are castrated before puberty have very little prostatic tissue so you may be wondering considering castration to prevent prostate cancer or enlargement? It is also believed that without the male hormone testosterone that is produced within the testicles, the prostate gland does not develop. If we were to surgically explore this area in one of these dogs, only a tiny bulge would be noted in the urethra. The small size causes no harm to the dog, since the only known purpose of the prostate is support and nourishment of the sperm cells. If a mature dog is castrated, the gland will shrink to less than one-fourth of its previous size. Within a few months, its useful cells will cease all or nearly all production of the helpful fluids so this is the ideal of the medical community in the twentieth century in the Charles Huggins era but now the rhythm has change!
Foundation of Testosterone and Prostate Cancer
The genesis for the panic that testosterone therapy upsurges the risk of prostate cancer initiated with the work of Charles B. Huggins, a urologist at the University of Chicago. Huggins we were told was initially concerned in the medical disorder called benign enlargement of the prostate, called benign prostatic hyperplasia (BPH), a patient Benjamin Franklin was told to have BPH and was endorsed with originating a tube he inserted through the urine passage to relieve the hindrance.
Interestedly, dogs appear to be the only sorts recognize of other than humans that naturally develop prostate conditions on a consistent basis. So at the turn of the twentieth century, Huggins began investigating on the effects of castration on BPH in dogs as reports emanate that castration was successful in treating men with severe obstruction from BPH but not only did the dogs' prostates shrink after castration, but Huggins made an added extensive remark.
In fact he observed that the microscopic appearance of prostates of some of these dogs contained areas that were indistinguishable from human prostate cancers. Even more significantly, after castration, dogs with these cancerous-appearing areas also demonstrated shrinkage of their prostates. Indeed, when their prostates were removed, the dogs had no further evidence of the cancerous-appearing areas which was interesting!
Huggins and his colleagues then use his dog results to humans we were told. By this time, it was known that the key effect of castration was to reduce testosterone levels in the blood. He took a group of men who had metastatic prostate cancer and lowered their testosterone levels, either by removing the testicles or by administering estrogen. A blood test called acid phosphatase was high in men with metastatic prostate cancer, and Huggins and his associates showed that acid phosphatase plunged substantially within days of lowering testosterone. Of even greater consequence for the future of testosterone therapy, Huggins also reported that administration of testosterone injections to men with prostate cancer caused acid phosphatase to rise. Huggins and his colleagues concluded that reducing testosterone levels caused prostate cancer to shrink and raising testosterone levels caused “enhanced growth” of prostate cancer.
His demonstration of the androgen dependency of prostate cancer was extremely significant, since until that time in the early 1940s prostate cancer was not curable. After lowering testosterone by castration or by estrogen became the normal management for advanced disease and remains a mainstay of treatment to this day. He was eventually awarded the Nobel Prize in 1966 for his work showing that prostate cancer grew or shrank depending on testosterone levels we were told. So he is the legend of testosterone and prostate cancer!
The Rhythm Change in modern era
However, although many patients initially respond to androgen depletion therapy, they almost invariably relapse and develop resistance with transition of the disease to a castration-resistant state. Over the past decade, the better understanding of the mechanisms that drive resistance to castration has led to the development of next-generation androgen receptor targeting agents such as abiraterone acetate and enzalutamide. Now there are over 100 articles that proved testosterone as a useless therapy for prostate cancer. The American Cancer Society says testosterone therapy does not cure prostate cancer and some even described it as useless therapy. You see unlike breast cancer and estrogen that has a strong link it is a different ball game with prostate cancer and testosterone. It is believed that high testosterone predispose men to prostate cancer but if it true just common sense could even come in here to say that young men in their 20s and 30's have high testosterone level and also men in Okinawa s if that is the case then these group of men should be more prone to prostate cancer but rather not. The issue here rather is low testosterone rather is the problem but not high testosterone.
(Jankowska 2009) Men with low estradiol levels had as much as a 50 percent lower survival compared with men who had mid-range levels of the female hormone. High estradiol levels were also associated with poorer survival.
This is the key problem, Estrogen dominance in men is the result of an imbalance between testosterone and estradiol. It occurs when testosterone levels are not sufficient to stop or balance the effects of estradiol. Men who carry extra weight/fat have higher estrogen levels because fat cells convert testosterone and androstenedione (a precursor of testosterone) into estrogen. When men develop estrogen dominance, they can actually experience some of the same symptoms that affect women, including weight gain and breast cell growth. Men who develop enlarged breasts have extra estradiol. Estrogen dominance (an imbalance of testosterone and estrogen) also stimulates benign prostate hypertrophy (BPH) and prostate cancer. In fact, estrogen dominance is believed to be a major contributing cause of prostate cancer and not testosterone high testosterone. Other causes of estrogen dominance include: insulin resistance, stress, personal care product, BPA, pesticides and herbicides, hormones from meat and dairy meat products, diet high in animal fat or excessive consumption of omega-6 fatty acids
Harvard-based Abraham Morgentaler, MD, FACS, has demonstrated this theory to be mistaken. Contrary to the notion that restoring testosterone to youthful levels is somehow risky, Dr. Morgentaler meticulously shows an increased risk of prostate cancer in aging men with low testosterone in the life extension magazine. Destroying the Myth about Testosterone Replacement and ...www.lef.org/Magazine/2008/...Testosterone...Prostate-Cancer/Page-01
According to the life extension magazine in this exclusive excerpt from his book, Testosterone for Life, Dr. Morgentaler recounts how it takes years, even decades, to correct a medical myth. In this case, the medical establishment's misconception about testosterone and prostate cancer has condemned millions of aging men to suffer degenerative diseases caused by testosterone deficiency.
The relationship of testosterone to prostate cancer has undergone a significant reevaluation, and all recent evidence has reinforced the position that testosterone therapy is safe for the prostate.
There are several reasons this theory regarding testosterone and prostate cancer is inaccurate, the first of which is due to a study that looked at the link between low testosterone and mortality.
A study, published in the Archives of Internal Medicine by the VA Puget Sound Health Care System and the University of Washington at Seattle, evaluated whether low testosterone levels are a risk factor for mortality in men over the age of 40. The participants all had their testosterone levels checked regularly during the study which lasted for five years.
The study discovered that men who were classified as having low testosterone had an 88% increased risk of death compared to the group who had normal testosterone levels.
Another study looked at the increased risk of fatal heart problems in relation to hormone therapy. The study was conducted in King's College London by epidemiologist Mieke Van Hemelrijck and looked through the records of 30,642 Swedish men with either locally advanced or metastatic prostate cancer who had received prostate cancer hormone therapy as the primary treatment.
The study compared the rates of heart problems among these patients with the general Swedish population. The study found that “prostate cancer patients treated with hormone therapy had an elevated risk of developing all of the individual types of heart problems and that they were more likely to die from those causes”.
Beyond this, the study found that heart problems had started in the patients within months of beginning their hormone therapy.
This lead to hormone therapy being declared medically useless: the American Cancer Society says that "Hormone therapy does not cure prostate cancer.
There are several reasons this theory regarding testosterone and prostate cancer is inaccurate said Abraham Morgentaler, according to him , Huggins himself state that administration of testosterone to men caused “enhanced growth” of prostate cancer in men with metastatic disease. A second was a well-known 1981 article from the Memorial Sloan Kettering Cancer Institute in New York, authored by the most prominent prostate cancer expert of his era, Dr. Willet Whitmore that reported near-universal poor outcomes when men with metastatic prostate cancer received testosterone injections. And the third was the phenomenon known as testosterone flare. Testosterone flare refers to the temporary increase in testosterone caused by the use of medications called LHRH agonists in men with advanced prostate cancer. Testosterone flare has been associated with a variety of complications attributed to the sudden growth of prostate cancer.
All three of these issues applied only to men with known metastatic disease, and because no one was suggesting that testosterone therapy be offered to men with advanced prostate cancer, the existence of this literature wasn't terribly troubling. What was of concern to those medical officers prescribing testosterone therapy was the possibility that they might be putting our otherwise healthy patients at risk for prostate cancer, but so far all the data looked reassuring on this point. Metastatic disease was something quite different, and it would not have been shocking to learn that it responded differently to high levels of testosterone than localized disease within the prostate.
He found the original article by Huggins from 1941. It was in the very first published volume of what is now a highly respected journal called Cancer Research. he read how Dr. Huggins and his coinvestigator, Clarence Hodges, used the new blood test called acid phosphatase to show that lowering testosterone by castration or estrogen treatment caused prostate cancer to regress, and how T injections had caused “enhanced growth” of prostate cancer in these men. And then he noticed something that made his heart race.
Huggins and Hodges had written that three men had received T injections. But results were given for only two men. And one of these men had already been castrated. This meant that there were results for only a single man who had received T injections without prior hormonal manipulation. Dr. Huggins had based his “enhanced growth” conclusion on a single patient, using a test—acid phosphatase—that has since been abandoned because it provides such erratic results!
He sat there in the basement of the library, reading the same lines over and over to make sure he hadn't misread it. Later, he asked several colleagues to read it as well. Dr. Huggins's assertion that higher testosterone caused greater growth of prostate cancer, repeated for so long and accepted as gospel, was based on almost nothing at all! Because there was a bothersome unresolved paradox to explain. For decades, the storyline was that lowering testosterone levels caused prostate cancer to shrink away and raising testosterone levels caused it grow. The second part of this story was now seriously in doubt, yet the first part was obviously correct. In his own practice, he had seen the beneficial effects of lowering testosterone levels many times over in men with advanced prostate cancer. This part of Dr. Huggins's work was indisputable. But if lowering testosterone levels caused these cancers to shrink, how was it possible that raising testosterone levels did not cause the cancers to grow? This was a paradox that needed to be solved if physicians were to accept the possibility that testosterone therapy may not increase the risk of prostate cancer.
The answer turns out to be not all that complicated. All the reports of testosterone causing rapid growth of prostate cancer occurred in men who already had extremely low testosterone levels, due to castration or estrogen treatment. Once they get beyond the near-castrate range, it is hard to find any evidence that changes in T concentrations matter at all to prostate cancer. This is essentially what Drs. Fowler and Whitmore described in their 1981 article when they suggested that “near maximal” growth of prostate cancer is provided by naturally occurring T concentrations.
The experimental proof of this concept was provided by a landmark article published in 2006 using much more sophisticated means. In this study by Leonard Marks and colleagues, men with low testosterone received injections of testosterone or a placebo every two weeks for a total of six months. At the beginning and end of the study, measurements of testosterone and DHT (the more active form of testosterone within prostate tissue) were obtained from the blood and also from the prostate itself. The results showed that although blood concentrations of testosterone and DHT rose substantially in the T injection group, as expected, the concentration of testosterone and DHT within the prostate itself did not change at all and was similar to the group that received placebo injections. In addition, biochemical markers of prostate cell growth also did not change with T injections.
This study showed in elegant fashion that raising testosterone levels in the blood did not raise testosterone levels within the prostate. It is as if once the prostate has been exposed to enough testosterone, any additional testosterone is treated as excess and does not accumulate in the prostate. In technical terms, we say the prostate has been saturated with regard to testosterone. And it is this saturation that resolves the paradox of testosterone and prostate cancer.
Saturation explains the paradox in this way. At very low levels of T, near the castrate range, prostate growth is very sensitive to changes in T concentration. Thus, severely lowering testosterone will definitely cause prostate cancer to shrink; adding testosterone back will cause the cancer to regrow. However, once we get above the point where the prostate is saturated with testosterone, adding more testosterone will have little, if any, further impact on prostate cancer growth. Experimental studies suggest the concentration at which this saturation occurs is quite low.
In other words, the old analogy he learnt in training was false. Testosterone is not like food for a hungry tumor. Instead, a much better analogy is, “Testosterone is like water for a thirsty tumor.” Once the thirst has been satisfied, prostate tumors have no use for additional testosterone. And the vast majority of men with low testosterone appear to have prostates that are not particularly thirsty.
Dr. Raphael NyarkoteyObu :ND(TAP00396)
Integrative Oncologist
MSc Prostate Cancer
Sheffield Hallam University, UK
Director of Men's Health Foundation Ghana
Tel: 0541090045
E. mail:[email protected]




 Minority will expose the beneficial owners of SML, recover funds paid to company...
Minority will expose the beneficial owners of SML, recover funds paid to company...
 Prof. Opoku-Agyemang has ‘decapitated’ the NPP’s strategies; don’t take them ser...
Prof. Opoku-Agyemang has ‘decapitated’ the NPP’s strategies; don’t take them ser...
 Abubakar Tahiru: Ghanaian environmental activist sets world record by hugging 1,...
Abubakar Tahiru: Ghanaian environmental activist sets world record by hugging 1,...
 Prof. Naana Opoku-Agyemang will serve you with dignity, courage, and integrity a...
Prof. Naana Opoku-Agyemang will serve you with dignity, courage, and integrity a...
 Rectify salary anomalies to reduce tension and possible strike action in public ...
Rectify salary anomalies to reduce tension and possible strike action in public ...
 Stop all projects and fix ‘dumsor’ — Professor Charles Marfo to Akufo-Addo
Stop all projects and fix ‘dumsor’ — Professor Charles Marfo to Akufo-Addo
 Blue and white painted schools will attract dirt shortly – Kofi Asare
Blue and white painted schools will attract dirt shortly – Kofi Asare
 I endorse cost-sharing for free SHS, we should prioritise to know who can pay - ...
I endorse cost-sharing for free SHS, we should prioritise to know who can pay - ...
 See the four arsonists who petrol-bombed Labone-based CMG
See the four arsonists who petrol-bombed Labone-based CMG
 Mahama coming back because Akufo-Addo has failed, he hasn't performed more than ...
Mahama coming back because Akufo-Addo has failed, he hasn't performed more than ...
