This paper focuses on temporal seed brachytherapy to give Ghanaian men a clear understanding of the patient cancer journey. Temporary brachytherapy, also known as high dose-rate (HDR) brachytherapy, involves inserting a source of high dose-rate radiation into the prostate gland for a few minutes at a time to destroy cancer cells. It is not available at every treatment center in the UK.
During the past decade, prostate seed implantation has been increasingly used as monotherapy or in combination with external beam radiotherapy (EBRT).1-4 Exponential growth has been forecasted so that while only 4% of men diagnosed with prostate cancer in 1996 were treated with brachytherapy, it is estimated that approximately half of the men diagnosed in 2006 will be implanted.5 A 1999 Medicare utilization review estimated that brachytherapy may eventually supplant prostatectomy as the treatment of choice for localized prostate cancer.
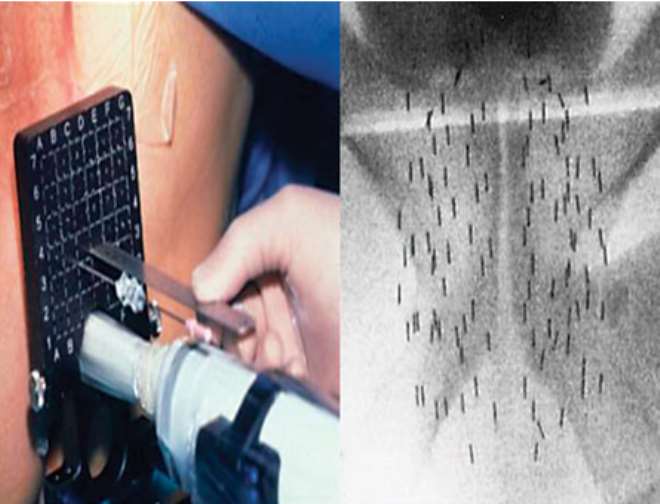
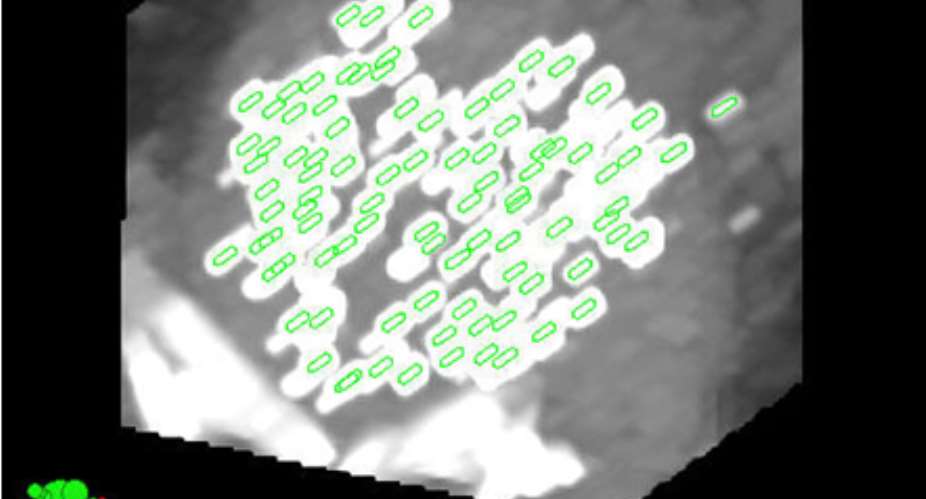
While the majority of prostate interstitial brachytherapy is performed with permanent seed implants, the use of a different implant technique known as temporary high dose-rate (HDR) brachytherapy has been increasing. During an HDR implant, small flexible needles are inserted through the perineum (the skin between the testicles and rectum) and a high dose of radiation is delivered to the prostate gland using a computer guided radioactive Iridium wire.
HDR brachytherapy provides many advantages including treatment optimization, accurate dose delivery, and radiation protection. Certain patients who are not good candidates for permanent seed implant may be better treated with HDR. Nevertheless, because the awareness of the HDR technique is not widespread, patients are often not offered this option. The intent of this article is to describe the procedure, its possible advantages over permanent seed implant, and the growing body of long-term results so that patients can include this modality when considering options for local PC therapy
You may be suitable for this treatment if your cancer is thought to be contained within the prostate gland (localised prostate cancer) and is 'medium risk'. Your cancer may be described as medium risk if:
your PSA level is between 10 and 20 ng/ml, or
your Gleason score is 7, or
the stage of your cancer is T2b or T2c.
Some men whose prostate cancer is beginning to spread to the area just outside the prostate (locally advanced prostate cancer), or with higher Gleason scores, may be able to have temporary brachytherapy. Check with your doctor or nurse.
You may have this treatment on its own or you may have it together with external beam radiotherapy and/or hormone therapy.
Advantages and disadvantages
Advantages
Treatment in hospital with temporary brachytherapy takes just one or two days.
It delivers a high dose of radiation direct to the prostate gland so healthy tissue nearby only gets a small dose of radiation and therefore is less likely to be damaged and cause side effects.
Recovery is quick, which means you can usually return to your normal activities within a week of treatment.
Disadvantages
It can cause side effects such as urinary, bowel and erection problems.
You will need a general or spinal anaesthetic. See the section 'What does treatment involve?'
If you require more than one radiation treatment you may need to stay in bed for at least six hours between treatments whilst the tubes are in your prostate. Some men find this very uncomfortable. See the section 'What does treatment involve?'
You may need to stay in hospital overnight.
It may be some time before you will know whether the treatment has been successful.
Treatment Pathway
It is likely that you will have a general anaesthetic so that you are asleep during the procedure. Another option is to have a spinal or epidural anaesthetic, so that you are awake but cannot feel anything. The specialist team will discuss the different options with you.
The specialist passes thin plastic or metal tubes through the area of skin between your testicles and opening of the back passage (perineum) into the prostate gland and the surrounding tissues. You will then have a computerised tomography (CT), magnetic resonance (MRI) or ultrasound scan. This allows the specialist to plan the doses of radiation needed for your treatment.
You may have your treatment while you are still under anaesthetic, or you may have it once you have woken up. During treatment, flexible tubes from the brachytherapy machine are attached to each of the tubes that are inside you. A highly radioactive pellet then travels down each of the tubes in turn. You may have just one treatment or you may have two or three treatments in total.
You will have a follow-up appointment a few weeks after your treatment, to check your PSA level and discuss any side effects. You will have regular appointments after that to monitor your PSA level and any side effects. If your treatment has been successful, your PSA level should drop.
Side effects of Temporal Brachytherapy
The most common side effects include tiredness, problems passing urine, erection problems, and bowel problems. These will affect each man differently, and you may not get all of the side effects.
Some men who have temporary brachytherapy and external beam radiotherapy together find that they have worse side effects. If you already had urinary, erection or bowel problems before treatment, these may be worse after treatment.
Questions you need to ask before commencing the Procedure
Will I have external beam radiotherapy before or after temporary brachytherapy?
Do I need hormone treatment before and/or after temporary brachytherapy?
What are the chances of side effects such as urinary problems, erection problems and bowel problems with this treatment?
How many treatments will I have? Will I be asleep or awake during treatment?
How long will I need to stay in hospital for the treatment?
How will we know if the treatment has worked?
What should my PSA level be after treatment and how often will you measure it?
If my PSA continues to rise, what other treatments are available?
About the Author
RAPHAEL NYARKOTEY OBU: ND
Registered Naturopathic doctor/Prostate Cancer expert
MSc Prostate Cancer
Sheffield Hallam University, UK
CEO DE MEN'S CLINIC & PROSTATE RESEARCH LAB,
MEN'S HEALTH FOUNDATION GHANA, DODOWA-AKOTO HOUSE
TEL: 0541090045
Reference
Temporal seed brachytherapy
prostatecanceruk.org/information/prostate-cancer/treatment/.../cryotherap..
Updated: Nov 2012 | Due for Review: Nov 2014
Temporary Seed Implant with High Dose Rate Brachytherapy
prostate-cancer.org/temporary-seed-implant-with-high-dose-rate-brachyt...
 2014-10-23 143338
2014-10-23 143338
 2014-10-23 143447
2014-10-23 143447




 Cecilia Dapaah: Reasons behind AG’s advice to EOCO not grounded in law – Martin ...
Cecilia Dapaah: Reasons behind AG’s advice to EOCO not grounded in law – Martin ...
 NPP should have reported Kingsley Nyarko’s conduct to police – Inusah Fuseini
NPP should have reported Kingsley Nyarko’s conduct to police – Inusah Fuseini
 Akufo-Addo cuts sod for MIIF Technical Training Centre
Akufo-Addo cuts sod for MIIF Technical Training Centre
 NPP didn’t struggle to win Ejisu by-election – Samuel Ayeh-Paye
NPP didn’t struggle to win Ejisu by-election – Samuel Ayeh-Paye
 A/R: Achiase Chief arrested for acid attack on community members
A/R: Achiase Chief arrested for acid attack on community members
 Naa Ayemoede returns to school
Naa Ayemoede returns to school
 Dadieso residents block Accra-Kumasi highway
Dadieso residents block Accra-Kumasi highway
 Kasoa soldier killer remanded
Kasoa soldier killer remanded
 Rashid Pelpuo slams Opoku Prempeh for denying dumsor
Rashid Pelpuo slams Opoku Prempeh for denying dumsor
