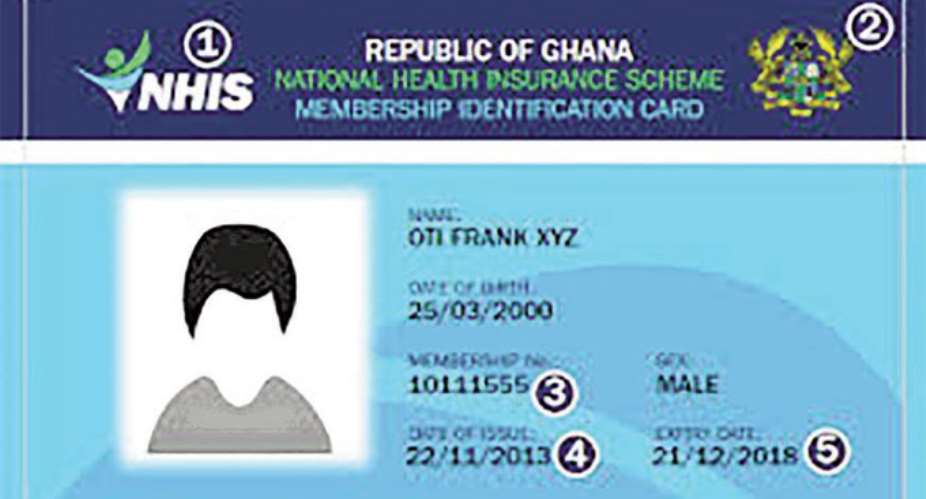
The National Health Insurance Scheme (NHIS) is one of the most significant social intervention programmes that have been initiated in Ghana since independence.
The level of patronage of the NHIS is good and could serve as an effective social healthcare policy tool.
Indications are that, about 60 percent of Ghanaians (14.2 million) have registered under the scheme.
However, the operational experience of the NHIS over the past 12 years has highlighted some shortcomings in the sustainability of the scheme on account of the mismatch of the cost of the scheme and financial resources available, human resource capacity and the misalignment of the administrative, technical and legal set up of the scheme.
DAILY GUIDE's Jamila Akweley Okertchiri had the privilege of interviewing Kwamina Amoasi-Andoh who has special expertise in health insurance on how to make the NHIS work again.
With over 25 years of experience, Mr Amoasi-Andoh developed the first health insurance scheme during his tenure as the Chief Executive Officer, Ghana Healthcare Company, Social Security and National Insurance Trust, Accra, Ghana.
This scheme later led to the development of the National Health Insurance Authority (NHIA) and the National Health Insurance Scheme (NHIS).
He has further developed multiple schemes, management systems and has currently come out with strategies to address the current problems facing the NHIA and NHIS.
Genesis
In 2001, the government decided to introduce a National Health Insurance Scheme (NHIS) in Ghana.
The government finally passed the National Health Insurance Act, 2003 (Act 650) in 2013 to secure the provision of basic healthcare services to persons resident in the country through mutual and private health insurance schemes, to put in place a body (the National Health Insurance Council) to register, license, and regulate health insurance schemes and to accredit and monitor healthcare providers operating under health insurance schemes, to establish a national health insurance fund that will provide subsidy to licensed district mutual health insurance schemes, to impose a health insurance levy and to provide for purposes connected with these.
Are There Any Loopholes In The Act?
The National Health Insurance Act, 2003 (Act 650) sidelined all the employer-worker schemes and the local and community initiatives because the act made the District Mutual Health Insurance Schemes (DMHIS) more or less compulsory and more attractive to residents in the districts to join than the private mutual or commercial schemes which were also permitted by the act.
Currently, the National Health Insurance Authority (NHIA) Act 852 of 2012 exists as the 'Authority' and 'Implementer' of one centralised National Social Health Insurance Scheme (NSHIS), establish a National Health Insurance Fund to pay for the cost of healthcare services to members of the scheme, establish private health insurance schemes and to provide for related matters in the country.
How Has That Reflected In The Implementation Of The Scheme?
Undoubtedly, NHIA is facing all the usual administrative, financial and operational challenges of social health insurance organisations the world over.
Our situation is compounded by the unique challenges of our social, political, economic, demographic and gender challenges. Hence, the 'Objects of the Authority' have not been met and, in fact, cannot be achieved under current conditions.
The current structural set up of NSHIS will never achieve self-financing and commercial viability and sustainability because of the mismatch of the cost of the scheme and the financing sources available to the scheme.
Projecting forward, the financial situation worsens when factors in the demographic trends of the population, the ever-growing informal economy; the planned introduction of the 'one-time-premium' payment programme which was not going to be possible in our circumstances. Introducing a one-time premium to an already underfunded scheme only made matters worse for the management of the scheme. The 'one-time-premium' idea is utopian and cannot be functionally implemented.
Also, our inability to vary premiums for the different category of subscribers of the scheme- unable to practise Premium Price Discrimination.
The NSHIS will have to be supported with funds from central government because the organisational and operational set up of the scheme is unnecessarily bureaucratic, inefficient and costly. For example, even those in the formal sector who were operating their viable schemes already can and are willing and able to pay more (higher premiums) for healthcare are not encouraged to do so under the present scheme.
So How Do We Make It Work Again?
The primary objective of all the national health insurance initiatives in Ghana has been to find a replacement for the 'cash-and-carry' healthcare financing.
We need to fashion out various health insurance schemes that meet the healthcare needs of the different social, demographic, geographical, gender and income classes across the country, with due cognisance of the respective funding sources and financial implications of each scheme, just as is done all over the world.
We can achieve this in Ghana by developing a strategy to transform the mandate and workings of NHIA and the decentralised NSHIS over three years to make them more efficient and relevant to providers and subscribers.
My initial suggestions are that we delink the operational and regulatory functions of the NHIA as it exists now and let NHIA focus on promoting and regulating the healthcare insurance industry in Ghana efficiently.
It should also establish and monitor treatment protocols, drug list, tariffs for provider's services and facilities, monthly or annual insurance premiums and related benefit package of the various schemes.
How Do You Mean?
Operationally, we should have three main types of health insurance schemes in the country to be operated by various private and public sector organisations that will cover all the relevant sectors as follows:
National Social Health Insurance Scheme (NSHIS) should be redefined and reorganised and managed by professional administrators from the districts/municipal /metropolitan areas.
This will serve as the basic safety net social healthcare scheme of the government offering primary care to all citizens, regardless of their ability to pay.
Membership to the schemes would be limited to residents of districts and rural communities; pregnant women, children and other identified vulnerable groups within the informal economy who cannot be tracked easily through a regular PAYE system.
Because the NSHIS scheme will serve as the basic 'safety net for all', it should be subsidised with public funds such as the NHIS Levy in addition to the basic premium contribution by members.
A well-structured organisational scheme and health delivery programmes targeting the informal economy and the vulnerable citizens would also attract the interest and attention of various donor groups that operate targeted healthcare interventions for the poor.
NHIA could perform certain clearing-house and central administrative and settlements functions for the NSHIS on account of fiscal and technical support that it would receive from the central government.
What Happens To National Mutual Health Insurance Schemes?
National Mutual Health Insurance Schemes should be encouraged to be set up as special purpose vehicles (SPV) or non-profit companies limited by guarantee, with membership from largely the formal sector and organised groups of the economy whose premiums can be easily tracked through the PAYE system (employees of government and the private sector on regular salary whose premiums could be collected easily through the PAYE system and/or SSNIT).
This scheme will be self-financing and even make surpluses to be invested into the improvements in the healthcare delivery system and infrastructure development.
The scheme will be financed with the 2.5 percent contributions from SSNIT and basic monthly premium contributions from employers and employees.
Up to a maximum of five National Mutual Health Insurance (NHIS) companies operating and competing in all regions of the country are recommended.
What About The Private Commercial Health Insurance Schemes?
The schemes that are currently operating 'unregulated' in the country should be encouraged and brought under the regulatory oversight of NHIA and the National Insurance Commission (if need be, for their financial stability).
These private schemes are generally profit-oriented business that target high net-worth and corporate executives/organisations and expatriates.
There are currently about five main private local and foreign health insurance companies operating in Ghana; a clear indication of the attractiveness and profit potential in the health insurance business.
What Are The Merits Of Your Proposed Strategy?
- Healthcare delivery and financing becomes more efficient and sustainable as compared with the current centralised NSHIS which has become very bureaucratic, inefficient and very costly to operate.
- The entire national population will be covered under some type of health insurance scheme that will be well-managed and regulated by the NHIA.
- Only the vulnerable in society will be assisted by state funds through the National Health Insurance Levy, thereby, reducing the fiscal burden of healthcare on the national budget.
- Citizens who migrate from informal to the formal sector will automatically move to other schemes which are self-financing.
- Provide incentive for people in the informal sector to join the NMHIS or the private commercial schemes.
- The National Social Health Insurance Scheme (NSHIS) programme which is to be implemented by every district in Ghana will attract donor support for technical and financial assistance and will utilise the technical capabilities of the viable self-financing National Mutual Health Insurance Schemes (NMHIS).
- Local management of the NSHIS will create local forum for subscribers, providers and the healthcare management office (the scheme) to deliberate on efficient management systems.
- Premiums will be collected more efficiently by local motivated agents who can identify with training, the indigenes who cannot pay premiums.
- Same amount will be paid as premium for all the people in the informal economy who are neither members of the NMHIS nor the PCHIS: say GH¢5-10 per month per subscriber with flexible payment terms based on the period they receive high income.
The detailed strategy, plans and activities and the review of the NHIA Act will be done in six months to start the implementation of the New National Health Insurance Scheme (NHIS) which limits the NSHIS to the informal vulnerable sector, introduces the mutual HIS which are self-financing for the formal sector and supervise the private for profit CHIS to operate efficiently.
These three schemes will provide opportunity to fit the poor in the informal sector – NSHIS; the employers and their workers in the formal sector – NMHIS; and the top executives who need more expensive extra care -PCHIS.
By Jamila Akweley Okertchiri



 Saglemi Housing Project will not be left to rot – Kojo Oppong Nkrumah
Saglemi Housing Project will not be left to rot – Kojo Oppong Nkrumah
 Transport fares hike: GPRTU issue two-day ultimatum
Transport fares hike: GPRTU issue two-day ultimatum
 ARC endorses Alan as presidential candidate – Buaben Asamoa
ARC endorses Alan as presidential candidate – Buaben Asamoa
 Akufo-Addo appoints Kwasi Agyei as new Controller and Accountant-General
Akufo-Addo appoints Kwasi Agyei as new Controller and Accountant-General
 PNC dismiss reports of mass resignations
PNC dismiss reports of mass resignations
 PAC advocates for revenue collectors to be engaged on commission basis, not full...
PAC advocates for revenue collectors to be engaged on commission basis, not full...
 Genser Energy commissions 110km of natural gas pipeline at Anwomaso
Genser Energy commissions 110km of natural gas pipeline at Anwomaso
 Naa Torshie calls for tolerance, peace ahead of 2024 election
Naa Torshie calls for tolerance, peace ahead of 2024 election
 Asantehene commends Matthew Opoku Prempeh for conceiving GENSER Kumasi Pipeline ...
Asantehene commends Matthew Opoku Prempeh for conceiving GENSER Kumasi Pipeline ...
 Let’s do away with ‘slash and burn politics’ in Ghana — Dr Adutwum
Let’s do away with ‘slash and burn politics’ in Ghana — Dr Adutwum
