• Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected mosquitoes.
• In 2010, malaria caused an estimated 655 000 deaths, mostly among African children.
• Malaria is preventable and curable.
• Increased malaria prevention and control measures are dramatically reducing the malaria burden in many places.
• Malaria can decrease gross domestic product by as much as 1.3% in countries with high disease rates.
• Non-immune travelers from malaria-free areas are very vulnerable to the disease when they get infected.
________________________________________
According to the World malaria report 2011, there were 216 million cases of malaria and an estimated 655 000 deaths in 2010. Malaria mortality rates have fallen by more than 25% globally since 2000, and by 33% in the WHO African Region. Most deaths occur among children living in Africa where a child dies every minute of malaria and the disease accounts for approximately 22% of all childhood deaths.
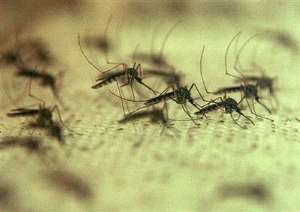
Malaria is caused by Plasmodium parasites. The parasites are spread to people through the bites of infected Anopheles mosquitoes, called "malaria vectors", which bite mainly between dusk and dawn.
There are four parasite species that cause malaria in humans:
• Plasmodium falciparum
• Plasmodium vivax
• Plasmodium malariae
• Plasmodium ovale.
Plasmodium falciparum and Plasmodium vivax are the most common. Plasmodium falciparum is the most deadly.
In recent years, some human cases of malaria have also occurred withPlasmodium knowlesi – a monkey malaria that occurs in certain forested areas of South-East Asia.
Transmission
Malaria is transmitted exclusively through the bites of Anopheles mosquitoes. The intensity of transmission depends on factors related to the parasite, the vector, the human host, and the environment.
About 20 different Anopheles species are locally important around the world. All of the important vector species bite at night. Anopheles mosquitoes breed in water and each species has its own breeding preference; for example some prefer shallow collections of fresh water, such as puddles, rice fields, and hoof prints. Transmission is more intense in places where the mosquito lifespan is longer (so that the parasite has time to complete its development inside the mosquito) and where it prefers to bite humans rather than other animals. For example, the long lifespan and strong human-biting habit of the African vector species is the main reason why more than 85% of the world's malaria deaths are in Africa.
Transmission also depends on climatic conditions that may affect the number and survival of mosquitoes, such as rainfall patterns, temperature and humidity. In many places, transmission is seasonal, with the peak during and just after the rainy season. Malaria epidemics can occur when climate and other conditions suddenly favour transmission in areas where people have little or no immunity to malaria. They can also occur when people with low immunity move into areas with intense malaria transmission, for instance to find work, or as refugees.
Human immunity is another important factor, especially among adults in areas of moderate or intense transmission conditions. Immunity is developed over years of exposure, and while it never gives complete protection, it does reduce the risk that malaria infection will cause severe disease. For this reason, most malaria deaths in Africa occur in young children, whereas in areas with less transmission and low immunity, all age groups are at risk.
Symptoms
Malaria is an acute febrile illness. In a non-immune individual, symptoms appear seven days or more (usually 10–15 days) after the infective mosquito bite. The first symptoms – fever, headache, chills and vomiting – may be mild and difficult to recognize as malaria. If not treated within 24 hours, P. falciparum malaria can progress to severe illness often leading to death. Children with severe malaria frequently develop one or more of the following symptoms: severe anaemia, respiratory distress in relation to metabolic acidosis, or cerebral malaria. In adults, multi-organ involvement is also frequent. In malaria endemic areas, persons may develop partial immunity, allowing asymptomatic infections to occur.
For both P. vivax and P. ovale, clinical relapses may occur weeks to months after the first infection, even if the patient has left the malarious area. These new episodes arise from "dormant" liver forms (absent in P. falciparum and P.malariae), and special treatment – targeted at these liver stages – is mandatory for a complete cure.
Who is at risk?
Approximately half of the world's population is at risk of malaria. Most malaria cases and deaths occur in sub-Saharan Africa. However, Asia, Latin America, and to a lesser extent the Middle East and parts of Europe are also affected. In 2010, malaria was present in 106 countries and territories.
Specific population risk groups include:
• young children in stable transmission areas who have not yet developed protective immunity against the most severe forms of the disease;
• non-immune pregnant women as malaria causes high rates of miscarriage (up to 60% in P. falciparum infection) and maternal death rates of 10–50%;
• semi-immune pregnant women in areas of high transmission. Malaria can result in miscarriage and low birth weight, especially during first and second pregnancies. An estimated 200 000 infants die annually as a result of malaria infection during pregnancy;
• semi-immune HIV-infected pregnant women in stable transmission areas, during all pregnancies. Women with malaria infection of the placenta also have a higher risk of passing HIV infection to their newborns;
• people with HIV/AIDS;
• international travellers from non-endemic areas because they lack immunity;
• immigrants from endemic areas and their children living in non-endemic areas and returning to their home countries to visit friends and relatives are similarly at risk because of waning or absent immunity.
Diagnosis and treatment
Early diagnosis and treatment of malaria reduces disease and prevents deaths. It also contributes to reducing malaria transmission.
The best available treatment, particularly for P. falciparum malaria, is artemisinin-based combination therapy (ACT).
WHO recommends that all cases of suspected malaria be confirmed using parasite-based diagnostic testing (either microscopy or rapid diagnostic test) before giving treatment. Results of parasitological confirmation can be available in a few minutes. Treatment solely on the basis of symptoms should only be considered when a parasitological diagnosis is not possible. More detailed recommendations are available in the Guidelines for the treatment of malaria.
Drug resistance
Growing resistance to antimalarial medicines has spread very rapidly, undermining malaria control efforts.
When treated with an artemisinin-based monotherapy, patients may discontinue treatment prematurely following the rapid disappearance of malaria symptoms. This results in incomplete treatment, and such patients still have persistent parasites in their blood. Without a second drug given as part of a combination (as is done with an ACT), these resistant parasites survive and can be passed on to a mosquito and then another person. Such monotherapies are therefore one of the primary forces behind the spread of artemisinin resistance.
If resistance to artemisinins develops and spreads to other large geographical areas, as has happened before with chloroquine and sulfadoxine-pyrimethamine (SP), the public health consequences could be dire, as no alternative antimalarial medicines will be available for at least five years.
WHO recommends the routine monitoring of antimalarial drug resistance, and supports countries to strengthen their efforts in this important area of work.
More comprehensive recommendations are available in the Global Plan for Artemisinin Resistance Containment (GPARC).
Prevention
Vector control is the main way to reduce malaria transmission at the community level. It is the only intervention that can reduce malaria transmission from very high levels to close to zero.
For individuals personal protection against mosquito bites represents the first line of defence for malaria prevention.
Two forms of vector control are effective in a wide range of circumstances.
Insecticide-treated mosquito nets (ITNs)
Long-lasting insecticide impregnated nets (LLINs) are the preferred form of ITNs for public health distribution programmes. WHO recommends coverage for all at-risk persons; and in most places, the most cost effective way to achieve this is through provision of LLINs, so that everyone in high transmission areas sleeps under a LLIN every night.
Indoor spraying with residual insecticides
Indoor residual spraying (IRS) with insecticides is the most powerful way to rapidly reduce malaria transmission. Its full potential is realized when at least 80% of houses in targeted areas are sprayed. Indoor spraying is effective for 3–6 months, depending on the insecticide used and the type of surface on which it is sprayed. DDT can be effective for 9–12 months in some cases. Longer-lasting forms of IRS insecticides are under development.
Drugs can also be used to prevent malaria. For travellers, malaria can be prevented through chemoprophylaxis, which suppresses the blood stage of malaria infections, thereby preventing malaria disease. WHO recommends intermittent preventive treatment with sulfadoxine-pyrimethamine for pregnant women living in high transmission areas, during the second and third trimesters. Similarly, for infants living in high-transmission areas of Africa, 3 doses of intermittent preventive treatment with SP is recommended delivered alongside routine vaccinations.
Insecticide resistance
Much of the success to date in controlling malaria is due to vector control. Vector control is highly dependent on the use of pyrethroids, which are the only class of insecticides used on currently recommended ITNs or LLINs. Resistance to pyrethroids has emerged, especially Africa, although so far there have been only one or two cases of obvious control failure.
Currently there is a lack of alternative, cost-effective and safe insecticides. The development of new, alternative insecticides is a high priority, but is an expensive and long-term endeavour. Development of new insecticides for use on nets is a particular priority.
Detection of insecticide resistance should be an essential component of all national malaria control efforts to ensure that the most effective vector control methods are being used. The choice of insecticide for IRS should always be informed by recent, local data on the susceptibility target vectors.
Economic and health system impact
Malaria causes significant economic losses, and can decrease gross domestic product (GDP) by as much as 1.3% in countries with high levels of transmission. Over the long term, these aggregated annual losses have resulted in substantial differences in GDP between countries with and without malaria, particularly in Africa.
The health costs of malaria include both personal and public expenditures on prevention and treatment. In some heavy-burden countries, the disease accounts for:
• up to 40% of public health expenditures;
• 30% to 50% of inpatient hospital admissions;
• up to 60% of outpatient health clinic visits.
Malaria disproportionately affects poor people who cannot afford treatment or have limited access to health care, trapping families and communities in a downward spiral of poverty.
Elimination
Many countries – especially in temperate and sub-tropical zones – have been successful in eliminating malaria. The global malaria eradication campaign, launched by WHO in 1955, was successful in eliminating the disease in some countries, but ultimately failed to achieve its overall goal, thus being abandoned less than two decades later in favour of the less ambitious goal of malaria control. In recent years, however, interest in malaria eradication as a long-term goal has re-emerged.
Large-scale use of WHO-recommended strategies, currently available tools, strong national commitments, and coordinated efforts with partners, will enable more countries – particularly those where malaria transmission is low and unstable – to progress towards malaria elimination. In recent years, 4 countries have been certified by the WHO Director-General as having eliminated malaria: United Arab Emirates (2007), Morocco (2010), Turkmenistan (2010), and Armenia (2011).
Vaccines against malaria
There are currently no licensed vaccines against malaria or any other human parasite. One research vaccine against P. falciparum, known as RTS,S/AS01, is most advanced. This vaccine is currently being evaluated in a large clinical trial in 7 countries in Africa. Results will be emerging from this trial in 3 stages, and each set of results will be reviewed by external WHO advisory committees. A WHO recommendation for use will depend on the final results from the large clinical trial. Final results are expected in 2014 . Other malaria vaccines are at earlier stages of research.
WHO response
The WHO Global Malaria Programme is responsible for charting the course for malaria control and elimination through:
• forming evidence-based policy and strategy formulation;
• keeping independent score of global progress;
• developing approaches for capacity building, systems strengthening, and surveillance;
• identifying threats to malaria control and elimination as well as new areas for action.
WHO is also a co-founder and host of the Roll Back Malaria partnership, which is the global framework to implement coordinated action against malaria. The partnership mobilizes for action and resources and forges consensus among partners. It is comprised of over 500 partners, including malaria endemic countries, development partners, the private sector, nongovernmental and community-based organizations, foundations, and research and academic institutions.
Malaria deaths decline by 66% in Zambia
News release
23 APRIL 2009 | GENEVA/BRAZZAVILLE - Malaria deaths reported from health facilities in Zambia have declined by 66%. This result along with other supporting data indicates that Zambia has reached the 2010 Roll Back Malaria target of a more than 50% reduction in malaria mortality compared to 2000. On World Malaria Day, celebrated on 25 April, Zambia's efforts will be promoted as a model for other countries to follow. Rwanda, United Republic of Tanzania, and Sao Tome and Principe are the other African countries who have achieved major reductions in malaria mortality through accelerated malaria control activities.
The decline in Zambia was especially steep after 3.6 million long-lasting insecticidal nets were distributed between 2006 and 2008. During this period malaria deaths declined 47% and nationwide surveys showed parasite prevalence declined 53% from 21.8% to 10.2% and the percentage of children with severe anaemia declined 68% from 13.3% to 4.3%. Most moderate and severe anaemia in children is caused by malaria.
"This is a remarkable achievement and a tribute to the hard work and commitment of the Ministry of Health of Zambia and its partners to combat malaria," said Dr Luís Gomes Sambo, WHO Regional Director for Africa. "As we celebrate World Malaria Day this week, I urge all countries affected by malaria to intensify and sustain malaria control and elimination efforts in order to meet the 2010 goal of 100% coverage."
WHO, with the support of the Global Fund to fight AIDS, Tuberculosis and Malaria, has been collaborating with health ministries over the last two years to evaluate impact from accelerated malaria control activities.
Malaria control activities accelerated
Accelerated malaria control activities started in Zambia in 2003 when approximately 500 000 insecticide-treated nets were distributed and artemisinin-based combination therapy (ACT) started in seven pilot districts through a grant from the Global Fund.
Since then, the Ministry of Health of Zambia has further expanded malaria control activities with grants worth US$ 120 million from the Global Fund and support from partners including the President's Malaria Initiative (PMI), the Malaria Control and Evaluation Partnership in Africa (MACEPA) and the World Bank Booster Program for Malaria Control in Africa.
“The Global Fund is pleased to see proof that malaria control resources provided by the Ministry of Health, the Global Fund, and other partners are resulting in a dramatic reduction of preventable deaths,” said Dr Michel Kazatchkine, Executive Director of the Global Fund, which provides two thirds of all resources for malaria control worldwide. “Zambia stands as an example of what we can achieve throughout Africa through the combination of universal access to bednets and effective malaria medicines,” he said.
Increasing coverage
By 2006-2007, large amounts of insecticide-treated nets and ACT were distributed and indoor residual spraying was taking place in 15 of 72 districts in Zambia. During 2006 and 2007 insecticide-treated nets were distributed to the general population rather than only children and pregnant women, who were the primary beneficiaries in earlier campaigns.
Mr Kapembwa Simbao, Minister of Health for Zambia said the Government of Zambia is committed to increasing coverage of key malaria control interventions and reducing the burden of malaria throughout the country.
"We will endeavour to continue to build on progress made and ensure that malaria control is addressed as part of a health systems strengthening effort to ensure that ACTs will reach all persons with suspected malaria thereby ensuring universal coverage," he said.
In countries with moderate and low transmission malaria, it appears that the Roll Back Malaria target of a more than 75% reduction is within reach several years before 2015. Aggressive malaria control measures as in Zambia may enable African countries to make rapid progress towards the Millennium Development Goals target of reducing child mortality by two thirds by 2015
Malaria Consortium in Zambia
As an established member of the malaria community in Zambia, Malaria Consortium has formed strong ties with key partners. This allows work at provincial, district and health facility levels.
Malaria Consortium works in Zambia as a partner to the Ministry of Health, and most specifically, the National Malaria Control Centre. Programmes are carried out throughout Southern and Eastern Provinces. Malaria Consortium Zambia is supported by Irish Aid and has worked to strengthen the health system in Zambia since 2004
Malaria Consortium is currently operating in all 11 districts of Southern Province, and 8 districts of Eastern Province. The formation of District Malaria Task Forces has helped to coordinate malaria control activities by bringing together different organisations to provide improved healthcare. Key successes in Zambia include support to the Community Malaria Booster programme and support to the National Malaria Control Centre at various events to advocate for malaria.
Malaria Consortium has also been active in the roll out of Home Based Management of Fever (HBMF) which includes training of community health workers in the use of Rapid Diagnostic Tests to detect malaria and using treatment drugs of choice artemisinin based combination therapies (ACTs).
________________________________________
Activities
Malaria Consortium Zambia focuses on four main areas:
• Quality Assurance (QA): Under a partnership with Improving Malaria Diagnostics, Malaria Consortium is creating quality assurance guidelines and training curricula. Malaria Consortium plans to take the lead in the QA trainings throughout Southern and Eastern Provinces, and provide technical support for training programmes in the remaining seven Zambian provinces.
• Data Analysis: Malaria Consortium has made an impact in Zambia by providing comprehensive solutions for diagnosis, treatment and prevention. By conducting training for 57 district staff in Southern and Eastern Provinces on how to work with malaria data to reveal patterns in care, incidence and mortality, the organisation is moving forward to the next step - transferring management responsibilities to the districts themselves. Prior to the launch of this training programme, data mismanagement was a major problem but discrepancies are now disappearing to aid the group's overall efficiency.
• Malaria Task Forces : Instead of relying solely on the health care system to reduce malaria, Malaria Consortium has also tapped the potential of business, along with NGOs and other government ministries to reach further into local communities. The idea of a Malaria Task Force at the District level is based on the assumption that the public sector stands to benefit from the greater human and material resources that the private sector demands. The objectives for all Malaria Task Forces are the same: to involve stakeholders in the coordination, planning, implementation, advocacy, monitoring and evaluation, to reduce the burden of malaria by reducing incidences in all age groups.
• Case Management: Providing prompt, effective treatment for malaria remains an unmet goal for health centres across Zambia. In response to the debilitating human resource crisis in the Zambian health system, Malaria Consortium has designed a case management training that targets all levels of staff, to ensure that any staff member handling malaria cases knows the correct protocols. Malaria Consortium has invited doctors, clinical officers, nurses, and a host of other health staff to participate in the case management trainings.
• Projects Currently Undertaken in Zambia
•
Project Title Funding Organisation
Health Systems Strengthening Irish Aid
Community Based Fever Management CIDA
•




 Dumsor: Mathew Opoku Prempeh has been disrespectful, he should be fired – IES
Dumsor: Mathew Opoku Prempeh has been disrespectful, he should be fired – IES
 NPP prioritizing politics over power crisis solution — PR Strategist
NPP prioritizing politics over power crisis solution — PR Strategist
 E/R: Gory accidents kills 3 persons at Aseseaso, several others critically injur...
E/R: Gory accidents kills 3 persons at Aseseaso, several others critically injur...
 Nobody can come up with 'dumsor' timetable except Energy Minister – Osafo-Maafo
Nobody can come up with 'dumsor' timetable except Energy Minister – Osafo-Maafo
 Dumsor: You ‘the men’ find it difficult to draw timetable when ‘incompetent’ NDC...
Dumsor: You ‘the men’ find it difficult to draw timetable when ‘incompetent’ NDC...
 We’re working to restore supply after heavy rains caused outages in parts of Gre...
We’re working to restore supply after heavy rains caused outages in parts of Gre...
 NPP government plans to expand rail network to every region — Peter Amewu
NPP government plans to expand rail network to every region — Peter Amewu
 Dumsor must stop vigil part 2: We’ll choose how we demonstrate and who to partne...
Dumsor must stop vigil part 2: We’ll choose how we demonstrate and who to partne...
 2024 elections: NDC stands on the side of morality, truth; NPP isn't an option —...
2024 elections: NDC stands on the side of morality, truth; NPP isn't an option —...
 Akufo-Addo has moved Ghana from 'Beyond Aid' to ‘Beyond Borrowing’ — Haruna Idri...
Akufo-Addo has moved Ghana from 'Beyond Aid' to ‘Beyond Borrowing’ — Haruna Idri...
