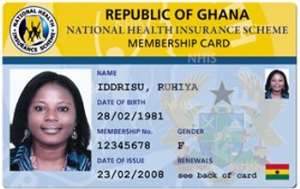
There have been various reports that point to the negative direction that the National Health Insurance Scheme (NHIS) is forever heading towards doom.
There have also been countless occasions that the NHIS Boss, Mr. Sylvester Mensah, had stepped to the defense of the scheme painting high-quality pictures of the scheme under his watch, in spite of the negative stories.
All these Public Relations tactics have done beneficiaries of the scheme more harm than good since they fail to provide proactive measures to make the scheme run proficiently.
From all indications, the scheme is indeed adrift the kind of quality being parried around by those so-called paid communicators of the scheme.
Weeks of painstaking investigations by your authoritative ModernGhana have uncovered massive extortion under the current National Health Insurance Scheme (NHIS) at the Pentecost Clinic within Kpasa, in the Volta Region of Ghana.
Discreet inquiries made by ModernGhana revealed that card-bearing patients of the NHIS were still being charged medical fees even before examination or treatment.
Authorities of the Kpasa Pentecost Clinic, who were not even ready to disclose their identities, revealed that the NHIA have not paid claims for over 7-months now hence they are not accepting the cards leading to grand extortion at the clinic.
Some of the victims who spoke to ModernGhana revealed that they are paying as much as GHC70 even though they have NHIS cards.
“Those who were not able to raise the funds have been turned away and as you can see, more patients are flooded here with NHIS Cards and the doctors and nurses are not even showing any sign of care,” a patient who only gave his name as Baaba Waheed told ModernGhana.
About The NHIS
NHIS in Ghana was conceived by former president John Kufuor who when seeking the mandate of the people in the 2000 elections, promised to abolish the cash and carry system of health delivery. Under the cash and carry system, the health need of an individual was only attended to after initial payment for the service was made.
Even in cases when patients had been brought into the hospital on emergencies it was required that money was paid at every point of service delivery.
Upon becoming president, former president Kufuor pushed through his idea of getting rid of “cash and carry” and replacing it with an equitable insurance scheme that ensured that treatment was provided first before payment. In 2003, the scheme was passed into law.
Under the law, there was the establishment of National Health Insurance Authority which licenses, monitors and regulates the operation of health insurance schemes in Ghana. Like many countries in the world, Ghana's health insurance was fashioned out to meet specific needs of its citizens.
The health insurance was set up to allow everybody to make contributions into a fund so that in the event of illness contributors could be supported by the fund to receive affordable health care. Under this policy, three types of health insurance schemes were set up. They were:
• The District-Wide Mutual Health Insurance Scheme.
• The Private Mutual Health Insurance Scheme.
• The Private Commercial Health Insurance Scheme.
In order for the system to function well, the government decided to support the District Mutual Health Insurance Scheme concept to ensure that:
• Opportunity is provided for all Ghanaians to have equal access to the functional structures of health insurance.
• Ghanaians do not move from an unaffordable 'Cash and carry' regime to another unaffordable Health Insurance one.
• A sustainable Health Insurance option is made available to all Ghanaians.
• The quality of health care provision is not compromised under Health Insurance.
Like all insurance schemes, different types of premiums are available under the country's NHIS. Contributors are grouped according to their levels of income. Based on the group a contributor may fall in, there is specific premium that ought to be paid.
This was done since the socio-economic condition scheme contributors is not the same and the contributions was to be affordable for all to ensure that nobody is forced to remain in cash and carry system.
This meant that contributions payable could vary from one district to the other as even the disease burden was also not the same in all the districts. To ensure that all citizens made some contribution to the scheme, a 2.5% Health Insurance Levy on selected goods and services was passed into law so that the money collected could be put into a National Health Insurance Fund to subsidize fully paid contributions to the District Health Insurance Schemes.
 NHIS Boss, Mr. Sylvester Mensah
NHIS Boss, Mr. Sylvester Mensah
 [2]NHIS
[2]NHIS




 Former Kotoko Player George Asare elected SRC President at PUG Law Faculty
Former Kotoko Player George Asare elected SRC President at PUG Law Faculty
 2024 elections: Consider ‘dumsor’ when casting your votes; NPP deserves less — P...
2024 elections: Consider ‘dumsor’ when casting your votes; NPP deserves less — P...
 You have no grounds to call Mahama incompetent; you’ve failed — Prof. Marfo blas...
You have no grounds to call Mahama incompetent; you’ve failed — Prof. Marfo blas...
 2024 elections: NPP creates better policies for people like us; we’ll vote for B...
2024 elections: NPP creates better policies for people like us; we’ll vote for B...
 Don’t exchange your life for wealth; a sparkle of fire can be your end — Gender ...
Don’t exchange your life for wealth; a sparkle of fire can be your end — Gender ...
 Ghana’s newly installed Poland train reportedly involved in accident while on a ...
Ghana’s newly installed Poland train reportedly involved in accident while on a ...
 Chieftaincy disputes: Government imposes 4pm to 7am curfew on Sampa township
Chieftaincy disputes: Government imposes 4pm to 7am curfew on Sampa township
 Franklin Cudjoe fumes at unaccountable wasteful executive living large at the ex...
Franklin Cudjoe fumes at unaccountable wasteful executive living large at the ex...
 I'll 'stoop too low' for votes; I'm never moved by your propaganda — Oquaye Jnr ...
I'll 'stoop too low' for votes; I'm never moved by your propaganda — Oquaye Jnr ...
 Kumasi Thermal Plant commissioning: I pray God opens the eyes of leaders who don...
Kumasi Thermal Plant commissioning: I pray God opens the eyes of leaders who don...
