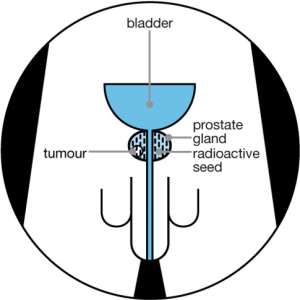
Many prostate cancers are being treated with radioactive seeds (brachytherapy).
The prostate gland is located under the bladder and in front of the rectum. It is vital that radiation therapy be focused in the prostate to avoid significant side effects. The prostate gland is also close enough to the skin that it can be easily reached by brachytherapy needles.
Brachytherapy is a type of radiotherapy, or radiation treatment, offered to certain cancer patients. There are two types of brachytherapy – high dose-rate (HDR) and low dose-rate (LDR). LDR brachytherapy is the type that is most commonly used to treat prostate cancer; it may sometimes be referred to as 'seed implantation' or it may also be called 'pinhole surgery'
Men may be suitable for this treatment if their cancer is thought to be contained within the prostate gland (localised prostate cancer) and:
PSA level is 10ng/ml or less, and
Gleason score is 6 or less, and
Stage of cancer is T1 - T2a.
In LDR brachytherapy, tiny radioactive particles the size of a grain of rice are implanted directly into the site of the tumour. These particles are known as 'seeds', and they can be inserted linked together as strands, or individually. Because the seeds are inserted or implanted directly into, or very close to, the tumour, they deliver high doses of radiation to the tumour without affecting the normal healthy tissues around it. This means that the procedure is less damaging than conventional radiation therapy, where the radioactive beam is delivered from outside the body and must pass through other tissues before reaching the tumour.
LDR prostate brachytherapy (seed implantation) is a proven treatment for early, localized prostate cancer (when the cancer is contained within the prostate). Under a general anaesthetic, the radioactive seeds are injected through fine needles directly into the prostate, so that the radiotherapy can destroy the cancer cells. The seeds are permanently implanted, so they remain in place but gradually become inactive as the radioactivity decays naturally and safely over time.
Unlike traditional surgery, LDR brachytherapy requires no incisions and is normally carried out as a day-case procedure. Sometimes a single overnight stay in hospital is required. Patients usually recover quickly from LDR brachytherapy, which means that most men can return to work or normal daily activities within a few days. As described below, LDR brachytherapy has a good side-effect profile with less risk of incontinence or impotence than other treatment options, and is becoming an increasingly popular alternative to major surgery (conventional radical prostatectomy or laparoscopic (keyhole surgery) radical prostatectomy).
Advantages
Men will be in hospital for just one or two days for the treatment.
Recovery is quick so most men can return to their normal activities a couple of days after treatment.
Men will have a shorter period of anaesthetic with brachytherapy compared with surgery as the procedure is quicker. This means you may recover more quickly from the anaesthetic.
The radiation is inside the prostate gland and does not travel far, so there may be less damage to the surrounding areas.
There may also be less damage to the blood vessels and nerves that control erections than after other prostate cancer treatments.
Disadvantages
Brachytherapy can cause side effects such as urinary, bowel and erection problems.
It requires one or two anaesthetics, depending on the method used. Anaesthetic can have side effects.
It may be some time before you will know whether the treatment has been successful.
What might be an advantage for one person may not be for someone else. You can talk to your doctor or nurse about your own situation.
Blood-stained urine or discoloured semen for a few days or weeks.
Bruising and pain in the area between your testicles and back passage which can spread to your inner thighs and penis. This will disappear in a week or two.
Discomfort when you pass urine and needing to pass urine more often, especially at night.
Problems passing urine, erection problems, bowel problems and tiredness.
Side effects will affect each man differently, and you may not get all of the side effects.
You will have a planning session to measure the size and position of your prostate to work out how many radioactive seeds you need. This is also a final check that the treatment is suitable for you. You may have a general anaesthetic so that you are asleep during the procedure, or you could have a spinal or epidural anaesthetic, so that you are awake but cannot feel anything.
The radioactive seeds will either be implanted on the same day as the planning session (one-stage procedure) or they will be implanted two to four weeks later (two-stage procedure). You will have a general anaesthetic or you may have a spinal or epidural anaesthetic.
You will have a computerised tomography (CT) or magnetic resonance imaging (MRI) scan four to six weeks after the treatment to check the position of the seeds. You will have regular follow-up appointments after this to monitor your PSA level and any side effects. If your treatment has been successful, your PSA level should drop, although it may start to rise again because your prostate will still produce some PSA. Some men may experience a rise and fall in PSA at around one to two years after treatment.
Questions to ask your doctor or nurse
Which type of permanent seed brachytherapy will I have? The one-stage or two-stage procedure?
Will I have external beam radiotherapy as well as brachytherapy?
What are the chances of side effects such as urinary problems, erection problems and bowel problems with this treatment?
How will I know if the treatment has worked?
What should my PSA level be after treatment and how often will you measure it?
If my PSA continues to rise, what other treatments are available?
What Does HDR Treatment for Prostate Cancer Involve?
This treatment frequently consists of a combination of three separate therapies:
High-dose-rate temporary brachytherapy
Moderate doses of Tomotherapy
Short-term hormonal therapy (optional)
This is a three-pronged attack against the cancer, also known as "triple therapy." Sometimes the doctor can omit the Tomotherapy (external beam radiation) or hormone therapy.
However, external beam radiation is often included because cancer cells may migrate outside the prostate gland, known as "extra-prostatic extension.” Treatments like a radical prostatectomy and permanent seed implant alone may miss cancer cells which have escaped outside the prostate into the surrounding tissues.
Scans like CT, MRI, ultrasound, and Prostascint may not detect cancer cells that have spread outside the prostate. Even though these scans may not show cancer spread beyond the prostate capsule, it can still be present. External beam radiation helps to target those areas surrounding the prostate gland. The probability that cancer has spread beyond the prostate gland can be estimated by the Partin tables.
The HDR Procedure
The HDR procedure can differ among hospitals. The radiation oncologist may insert 18- 25 catheters hollow plastic needles into the prostate gland. These are placed using anesthetic and rectal ultrasound guidance. After the needles are placed, a CT scan and a computer plan will calculate how long the radioactive source will stay in each needle. Three times over the following 24 hours, the needles are hooked up to the brachytherapy machine (HDR remote afterloader), and a treatment is given. During those 24 hours the patient will remain in a hospital bed.
The external beam component is given in a moderate dose, 4500 centigray divided over 4 weeks. This compares with the standard 8100 centigray divided over 9 weeks which would often be prescribed if the patient was having external beam radiation alone.
Many times, the radiation oncologist uses intensity modulated radiation therapy (IMRT) which does its own verification that the prostate is centered in the radiation field. The reduced dose and precision targeting of IMRT may result in a lower risk of side effects. Some patients may receive broader radiation fields if there is a possibility that their lymph nodes contain cancer.
HDR may also be used alone without any external beam radiation for early prostate cancer. This is known as "HDR monotherapy." If HDR is given without external beam, a higher dosage must be given, over 3 - 6 treatment fractions which may require two separate implants. There is not as much experience or results using HDR monotherapy as there is with using HDR plus external beam, so the combination treatment may be a more proven choice.
The radiation oncologist may also recommend short-term hormonal ablation therapy, which begins three months before the brachytherapy and continues for 3 - 12 months afterwards. The hormone therapy consists of a once-every-three-month injection of Lupron or Zoladex, and an antiandrogen medication like Casodex. The hormone therapy will shrink the cancer, shrink the prostate gland, reduce the PSA, and hopefully there will be less cancer cells for the brachytherapy to destroy.
Studies have shown that adding hormonal therapy to radiation can increase the tumor control rates, notably for Gleason 7 and higher tumors or PSA 10 or higher. Patients with an early prostate cancer may be recommended to take a shorter duration of hormone therapy, or none at all. Patients with high-risk prostate cancer may be recommended to take triple hormone blockade (Lupron + Casodex + Proscar) for approximately 15 months.
Who Can Have This Treatment?
HDR brachytherapy can be used for a wide range of prostate stages, PSA values, and tumor grades. The components and dosages are modified for those with low, intermediate, or high risk prostate cancer. This treatment can also be used for many tumors which are considered too advanced for radical prostatectomy. As long as there is no obvious spread to distant areas of the body, like the bones, this treatment may be considered. For early stages, treatment may be an alternative to the radical prostatectomy, but with fewer side effects.
What are the advantages and disadvantages?
The advantages and disadvantages of radiotherapy will depend on your age, health and the stage of your cancer. Your specialist team will discuss your individual situation and options with you.
Advantages
• Radiotherapy has none of the risks of surgery and having a general anaesthetic.
• It can be given when you are considered unsuitable or unfit for surgery.
• Some men may find the treatment position a bit uncomfortable but the radiotherapy itself is painless.
• It is relatively quick. Daily treatment sessions last about 10 to 20 minutes, and you do not need to stay in hospital overnight.
• You can carry on with many of your usual activities while you are having treatment.
Disadvantages
• You will need to go to a specialist hospital for treatment five days a week for several weeks -- and each visit could take at least an hour. This might be difficult if you need to travel a long distance.
• There is a risk of side effects including bowel problems, urinary problems and erectile dysfunction.
• It may be some time before you will know whether the treatment has been successful.
What does treatment involve?
You may be given hormone therapy for three to six months before you begin radiotherapy. This shrinks the prostate and makes the cancer easier to treat. You may also have further hormone therapy throughout your course of radiotherapy. Men who are at a higher risk of their cancer spreading may continue to have hormone therapy for at least two years after radiotherapy.
Before starting radiotherapy you will have scans to find the exact location, size and shape of your prostate. This is to make sure the treatment is accurate and that the surrounding areas do not receive more radiation than is necessary.
You will have one treatment at the hospital every day from Monday to Friday, with a rest over the weekend to help your healthy cells to recover. You can go home after each treatment session and will not have to stay overnight. Treatment normally lasts between seven and eight weeks.
At the beginning of each treatment, the radiographer will move you into the right position on the treatment couch. The treatment then starts and the machine moves around your body. It does not touch you and you will not feel anything. The whole session lasts about 10 to 20 minutes, including the time taken to position you on the treatment couch.
Your PSA level will be checked, usually six to twelve weeks after your treatment has finished. It will then be checked regularly, often at least every six months for two years, and after that at least once a year. This is to monitor how well the radiotherapy has worked.
If your treatment has been successful your PSA level should drop. However, how quickly this happens, and how low the PSA level falls, will depend on whether you had hormone therapy alongside radiotherapy. If you had radiotherapy on its own, it may take up to two years for your PSA level to fall to its lowest level. If you had hormone therapy as well, your PSA level may fall more rapidly.
What are the side effects?
Many men will get side effects during their treatment which only last a few weeks or months. However, some side effects can develop later and can become long term problems.
Possible side effects include bowel problems, urinary problems, tiredness and skin irritation. Longer term problems can include sexual problems and infertility. There is a small chance of other cancers developing, but this is very rare.
Side effects can often be treated, so if you have any unusual symptoms after having radiotherapy, ask your specialist team about it.
Questions to ask your doctor ?
- How many radiotherapy sessions will I have?
- Will I have hormone treatment? Will this continue after the radiotherapy?
- What side effects might I get? Will these be temporary or permanent?
- Will I be able to continue as normal during the treatment (for example, go to work)
- How will we know how successful the treatment has been?
- If the radiotherapy is not successful, which other treatments can I have?
- Who should I contact if I have any questions at any point during my treatment?
Recommendations for the first two months after seed implantation may include:
Avoiding sexual intercourse for two weeks
Using a condom during sexual intercourse in case a seed is passed during ejaculation
Limiting close contact with children and pregnant women
Not allowing children to sit on your lap for extended periods of time
Raphael Obu
Msc Prostate Cancer
Sheffield Hallam University, UK
CEO DE MENS CLINIC & PROSTATE RESAERCH LAB, DODOWA-AKOTO HOUSE
MENS HEALTH FOUNDATION GHANA
Registered and licensed Naturopathic Physician (TMPC Ghana)
References:
1. Prostate brachytherapy - Wikipedia, the free encyclopedia en.wikipedia.org/wiki/Prostate_brachytherapy . Accessed date last modified on 21 August 2013 at 14:35.
2. Prostate Cancer - Brachytherapy.com .www.brachytherapy.com/prostate-cancer.aspx
3. Permanent seed brachytherapy | Prostate Cancer UK prostatecanceruk.org/information/prostate-cancer/.../brachytherapy Updated: Nov 2012 | Due for Review: Nov 2014




 Meta releases new version of conversational AI across its platforms
Meta releases new version of conversational AI across its platforms
 Cape Town named Africa’s Best Airport 2024 by Skytrax
Cape Town named Africa’s Best Airport 2024 by Skytrax
 Bono East: Four injured after hearse transporting corpse crashes into a truck
Bono East: Four injured after hearse transporting corpse crashes into a truck
 ‘Be courageous, find your voice to defend our democracy’ — Sam Jonah urges journ...
‘Be courageous, find your voice to defend our democracy’ — Sam Jonah urges journ...
 Exodus of doctors, nurses and teachers have worsened because of unserious Akufo-...
Exodus of doctors, nurses and teachers have worsened because of unserious Akufo-...
 2024 election: Avoid insults, cutting down people in search of power – National ...
2024 election: Avoid insults, cutting down people in search of power – National ...
 ‘You passed through the back door but congratulations’ — Atubiga on Prof Jane Na...
‘You passed through the back door but congratulations’ — Atubiga on Prof Jane Na...
 Government’s $21.1 billion added to the stock of public debt has been spent judi...
Government’s $21.1 billion added to the stock of public debt has been spent judi...
 Akufo-Addo will soon relocate Mahama’s Ridge Hospital to Kumasi for recommission...
Akufo-Addo will soon relocate Mahama’s Ridge Hospital to Kumasi for recommission...
 We must not compromise on our defence of national interest; this is the time to ...
We must not compromise on our defence of national interest; this is the time to ...
